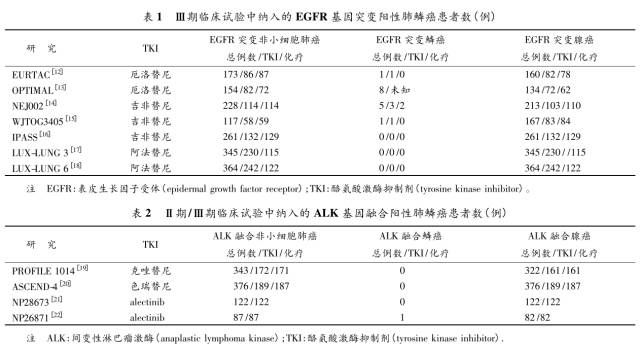
ALK阳性进展期非小细胞肺癌治疗的新探索
2017-10-26 周建英(浙江大学医学院附属第一医院呼吸与危重症医学科) 中华医学信息导报
2007年,日本学者Soda等首次报道从1例62岁吸烟的肺腺癌患者肿瘤组织中扩增出融合蛋白动物微管相关类蛋白4与间变性淋巴瘤激酶融合基因(EML4-ALK),并明确了该融合基因是肺癌的驱动基因之一。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ALK阳性#
77
#进展期#
91
#非小细胞#
65
#肺癌治疗#
81
学习了谢谢作者分享!
119
三代靶向药奥希替尼.
116
靶向治疗是当前NSCLC治疗的热点课题.进展很快.新药层出不穷.但耐药出现也快.三代EGFA_TKI可能是有希望的靶向药.
115
学习了新知识
102
学习了.谢谢分享!
161
学习了新知识
116