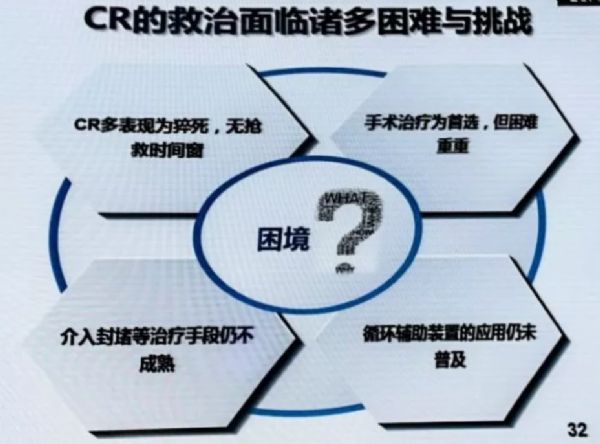
GW-ICC2017:急性心肌梗死合并消化道出血,如何选择止血方法?
2017-10-16 路人甲 医学界心血管频道
在第二十八届长城国际心脏病学会议上,首都医科大学附属北京安贞医院消化内科张杰教授带来了《急性心肌梗死合并消化道出血,如何选择止血方法》的精彩讲课,以下是小编整理的重要内容,分享给大家。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了
100
学习了
91
#止血#
74
#ICC#
59
#消化道#
52
#GW-ICC#
61
感谢分享
83
学习了提高了
76
学习了.谢谢
80
学习了谢谢分享!!
62