Arch Orthop Trauma Surg:肩袖预负荷对肱骨近端骨折骨折形态的影响:骨折模拟的概念验证
2022-08-16 医路坦克 MedSci原创
在手术训练方面,在人体身体标本上模拟逼真的肱骨近端骨折是重要的学习途径。本研究的目的是开发一种能够模拟真实的肱骨近端骨折的技术,并分析肩袖预载荷对产生的骨折形态的影响。
在手术训练方面,在人体身体标本上模拟逼真的肱骨近端骨折是重要的学习途径。
本研究的目的是开发一种能够模拟真实的肱骨近端骨折的技术,并分析肩袖预载荷对产生的骨折形态的影响。
材料与方法将10具身体标本(左侧6具,右侧4具)在自制的跌落试验台上折断,分成两组。5个标本在没有肩袖预紧力的情况下骨折,另5个标本在肩袖肌腱预加载2 kg的情况下骨折。肱骨干和缩短的肩胛骨被植入盆腔。采用外展90°、内旋10°的体位模拟高位手臂跌落动作。在每组的两个样本中,用高速视频成像记录骨折的出现。骨折前拍片评估三角骨结节指数作为骨密度的测量。骨折后进行X光和CT扫描以确定确切的骨折形态。骨折分类采用Neer分类。
结果10具身体标本均获得逼真的肱骨近端骨折。两组各有2例III型骨折和3例IV型骨折。肩袖肌预紧力对骨折形态无进一步影响。骨折模拟的高速视频显示,两组的骨折机制相同。我们观察到了一种两步骨折机制,最初头部部分撞击关节臼,随后头部和结节骨折,然后骨干进一步撞击肩峰,导致结节分离。
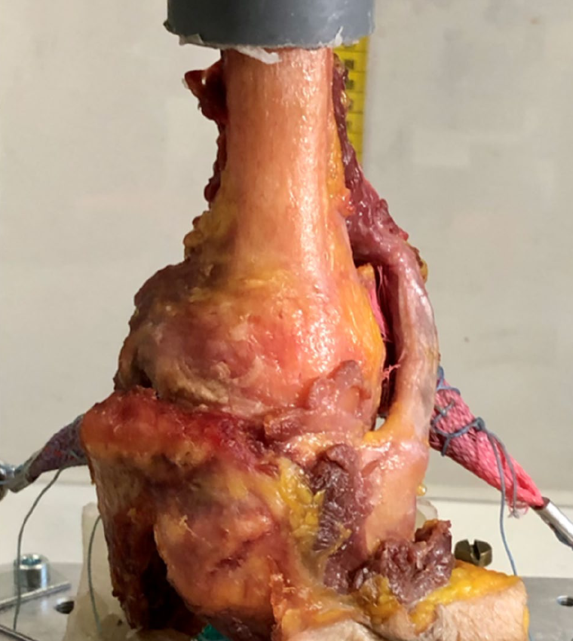
骨折模拟示意图:将肱骨远端和缩短的肩胛骨分别植入PMMA内。肱骨近端外展90°,内旋10°,肾盂水平放置。在每个肩袖肌腱(SSP/ISP/SSC)上植入指套和FiberWire。

A未加载标本和B标本预加载肩袖肌腱的高速图像。甲型和乙型头部破片的典型盾牌骨折特征
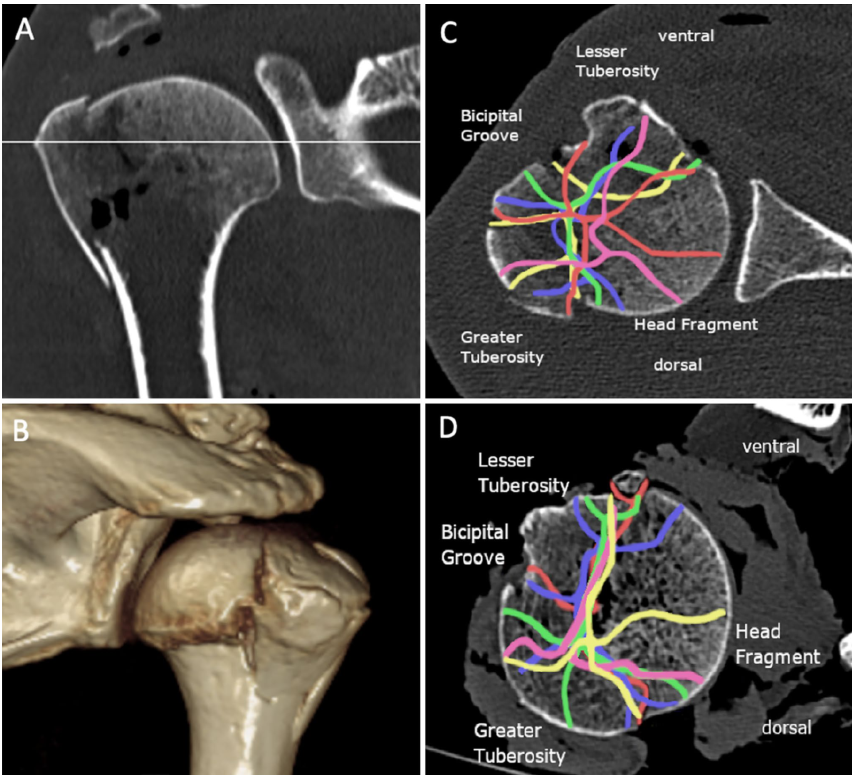
骨折线形态分析:A显示在大结节高度的标准化选层。B显示了裂缝形态的三维验证。C表示未加载组和骨折线,颜色不同于每个标本(软组织完全覆盖关节),D表示预加载组和骨折线形态,颜色与每个标本不同(软组织部分切除)
结论:高能轴向冲击能可靠地在身体标本上诱发逼真的肱骨近端骨折。肩袖肌肉的预紧力对初始骨折形态无影响。因此,我们可以将该技术用于现实生活中的外科教学。
文献来源: Lenz M, Kahmann S, Behbahani MInfluence of rotator cuff preload on fracture configuration in proximal humerus fractures: a proof of concept for fracture simulation.Arch Orthop Trauma Surg 2022 May 17;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Trauma#
82
#TRA#
78
#肱骨#
85
#近端#
102