Science:疟原虫感染宿主——与肝细胞的相互作用
2015-12-01 佚名 生物谷
美国传染病研究中心(Center for Infectious Disease Research)科学家们最近发现了关于疟原虫如何感染宿主这一谜题的一个关键环节。他们的工作最近发表于Science杂志,揭示了疟原虫如何入侵其最初目标器官——肝脏——的细节。如果不感染肝脏,疟原虫则无法繁殖或扩散到血液。血液感染会导致疾病、传播并最终死亡。 “这是一项重大发现,因为它揭示了疟原虫和它感染的人之间的
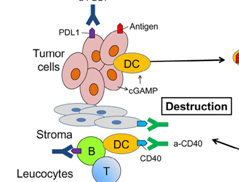
美国传染病研究中心(Center for Infectious Disease Research)科学家们最近发现了关于疟原虫如何感染宿主这一谜题的一个关键环节。他们的工作最近发表于Science杂志,揭示了疟原虫如何入侵其最初目标器官——肝脏——的细节。如果不感染肝脏,疟原虫则无法繁殖或扩散到血液。血液感染会导致疾病、传播并最终死亡。
“这是一项重大发现,因为它揭示了疟原虫和它感染的人之间的至关重要的相互作用。以前,我们对这种相互作用所知甚少。我们发现的分子细节将促进新药物和新疫苗的设计”传染病研究中心助理教授Alexis Kaushansky博士说道。

传染病研究所科学家解剖感染疟疾的蚊子。图片来源:传染病研究所
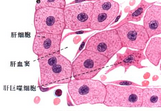
这项发现是Stefan Kappe博士实验室、Noah Sather博士实验室和Alexis Kaushansky博士实验室之间合作研究的结果。跨学科的结合、合作研究和技术方法使得这种类型的发现成为可能。正如美国国家卫生研究院疟疾细胞生物学部门主管Louis H. Miller所指出的:“这些关于肝脏受体EphA2作为疟原虫孢子体(sporozoite)入侵肝细胞靶点的发现是一个至关重要的进步,可能使得我们设计出阻止寄生虫感染的新策略。”
传染病研究中心已经开创了系统生物学方法进行研究,运用最先进的技术,培养科学家之间的合作,全面了解病原体和宿主之间的相互作用。这种方法为预防和治疗世界上最致命传染病所需的革命性进步提供了基本路径。
原始出处:
Researchers Uncover Essential Interaction Between Malaria Parasites and Liver Cells
Kaushansky A, Douglass AN,et al.Malaria parasites target the hepatocyte receptor EphA2 for successful host infection.Science. 2015 Nov 27;350(6264):1089-92.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#相互作用#
67
#肝细胞#
56
好东西,值得分享,学习了!
185
#SCIE#
55
#疟原虫#
67
#宿主#
53
#互作#
69
跨界成为成功的可能
151