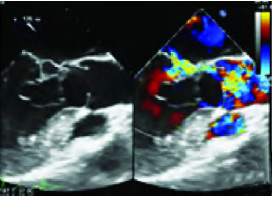
左心声学造影诊断二尖瓣血性囊肿1例
2019-04-03 何俊 何亚峰 吴洋 临床超声医学杂志
患者男,32岁,心脏杂音17年。现间断胸痛气短1年,胸痛呈绞痛样,持续约15min,休息后可好转,后频繁发作晕厥不适,每年发作3次,近来频发夜间阵发性呼吸困难。体格检查:体温36.6℃,脉搏60次/min,呼吸18次/min,血压110/67mmHg(1mmHg=0.133kPa)。心界向左下扩大,心尖部可闻及Ⅲ/6级收缩期吹风样杂音。



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血性囊肿#
55
#声学造影#
63
#囊肿#
67
#二尖瓣#
59
#造影#
63