棕色脂肪移植或可改善多囊卵巢综合征
2016-02-26 陈子江等 PNAS
近日,中科院动物研究所研究员金万洙研究组与山东大学生殖医学研究中心教授陈子江研究组合作,发现通过在多囊卵巢综合征(PCOS)模型大鼠体内移植外源性棕色脂肪组织(BAT)可显著激活内源性BAT,进而改善胰岛素抵抗,恢复规律性排卵,提高受孕率。该研究成果在线发表于2月22日的《美国科学院院报》。 根据前期研究,研究组设想能否通过增加PCOS模型大鼠体内BAT的量或激活内源性BAT来达到改善机体胰
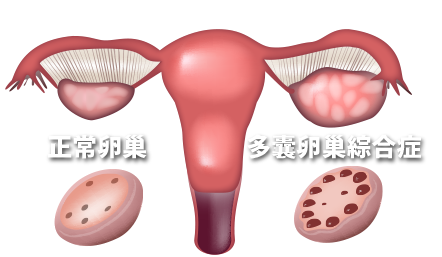
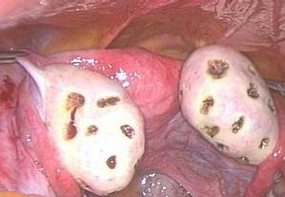
近日,中科院动物研究所研究员金万洙研究组与山东大学生殖医学研究中心教授陈子江研究组合作,发现通过在多囊卵巢综合征(PCOS)模型大鼠体内移植外源性棕色脂肪组织(BAT)可显著激活内源性BAT,进而改善胰岛素抵抗,恢复规律性排卵,提高受孕率。该研究成果在线发表于2月22日的《美国科学院院报》。
根据前期研究,研究组设想能否通过增加PCOS模型大鼠体内BAT的量或激活内源性BAT来达到改善机体胰岛素抵抗进而治疗PCOS的目的。 通过对PCOS模型大鼠BAT移植实验,验证了研究组的猜想。BAT移植改善了大部分的PCOS症状。进一步研究发现,通过对PCOS模型大鼠注射外源性脂联素,可获得与BAT移植类似的效果。该研究表明,BAT可能通过脂联素有效改善PCOS症状,为今后研究治疗提供了新的思路和靶点。
鉴于在多囊卵巢综合征患者身上很难实现棕色脂肪移植手术,他们目前在规划用能够激活棕色脂肪的小分子化合物进行大规模临床实验,以达到更好的治疗目的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#多囊卵巢#
52
哦
138
嗯嗯
142
哇
129
牛
175
厉害
126
很好好
19
#综合征#
51
白色脂肪棕色化,一个很有前景的领域
72