导语:丙肝疫苗,比我们想象的更重要。
丙型肝炎病毒(HCV)感染仍然是全世界最普遍的血源性病毒感染之一,同时也是全球传染病致死的主要原因。 尽管抗病毒疗法治愈率很高,但仍有超过7100万人患有慢性HCV感染,每年估计有175万例新感染和约40万人因此死亡。 从2009年到2018年,在阿片类药物注射增加的影响下,美国的HCV感染率增加了两倍。无法预防新的HCV感染是世界卫生组织2030年全球消除丙肝目标的主要阻碍。 预防性HCV疫苗将为通过中断传播实现消除目标提供重要工具。
研究人员利用黑猩猩腺病毒3(ChAd3)和修饰的牛痘安卡拉(MVA)载体(编码HCV基因型1b的非结构蛋白(NS))(ChAd3-NSmut和MVA-NSmut,GlaxoSmithKline)评估了异源性初始免疫-加强接种策略。 在第1阶段测试中,该疫苗方案具有临床可接受的安全性,并诱导了T细胞反应。
该试验的主要目的是评估ChAd3-NSmut和MVA-NSmut在高感染HCV感染者中的安全性,并确定预防慢性HCV的疫苗方案是否比安慰剂更有效防止感染。 该试验的次要目的是评估疫苗的免疫原性。
在此随机,双盲,安慰剂对照试验的1-2阶段中,我们评估了重组黑猩猩腺病毒3载体引发疫苗接种,然后进行了重组修饰牛痘安卡拉加强免疫; 两种疫苗均编码HCV非结构蛋白。 根据最近的注射吸毒史,被认为有HCV感染风险的成年人在第0和56天被随机分配(以1:1比例)接受疫苗或安慰剂。疫苗相关的严重不良事件 ,严重的局部或全身不良事件以及实验室不良事件是主要的安全终点。 主要疗效终点是慢性HCV感染,定义为持续病毒血症6个月。
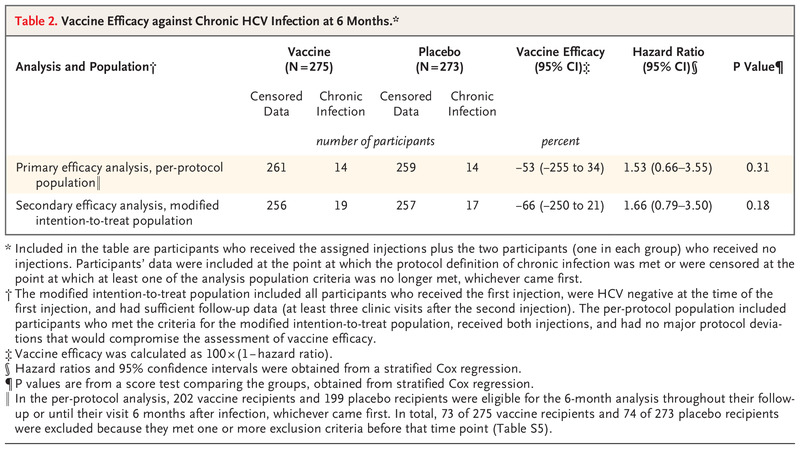
共有548名参与者接受了随机分组,每组274名。 两组之间慢性HCV感染的发生率无显着差异。 在按协议人群中,每组14名参与者发生了慢性HCV感染(危险比[疫苗与安慰剂]为1.53; 95%置信区间[CI]为0.66至3.55;疫苗效力为−53%; 95% [CI],-255至34)。 在改良的意向性治疗人群中,疫苗组的19名参与者和安慰剂组的17名参与者发生了慢性HCV感染(危险比,1.66; 95%[CI],0.79至3.50;疫苗功效,-66%; 95%[CI] ,-250至21)。疫苗组和安慰剂组之间感染后HCV RNA几何平均峰值水平有所不同(分别为每毫升152.51×103 IU和每毫升1804.93×103 IU)。在疫苗组的78%的参与者中检测到了针对HCV的T细胞应答。 两组中有严重不良事件的参与者百分比相似。
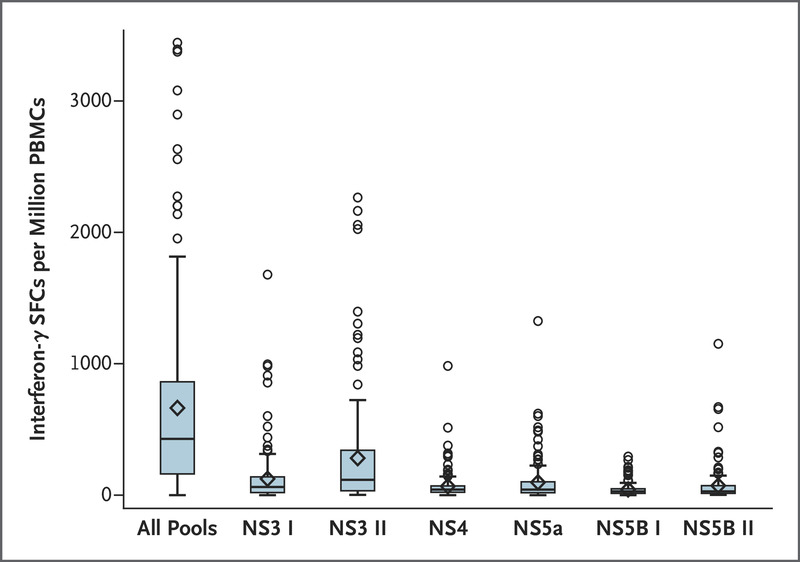
实验结果表明,在该试验中,HCV疫苗接种方案不会引起严重的不良事件,能够产生HCV特异性的T细胞反应,并降低了HCV RNA峰值水平,但并不能预防慢性HCV感染。
原文出处:https://www.nejm.org/doi/full/10.1056/NEJMoa2023345?query=featured_home
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#HCV#
85
#HCV感染#
75
学习了
91
好文章!
98
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
81