JCO:洛莫司汀联合化疗改善老年AML患者的生存?LAM-SA 2007全新结果公布
2018-11-20 肿瘤资讯编辑部 肿瘤资讯
老年AML患者在AML发病人群中占绝大多数,中位总生存期(OS)不到1年。一直以来,如何改善老年AML患者的不良预后始终为临床研究的热门话题。烷化剂洛莫司汀可通过调节DNA损伤修复起到显著的抗白血病效应,那么在传统化疗中联合洛莫司汀治疗是否改善预后?近日,JCO杂志发表了LAM-SA 2007临床试验最新结果。
老年AML患者在AML发病人群中占绝大多数,中位总生存期(OS)不到1年。一直以来,如何改善老年AML患者的不良预后始终为临床研究的热门话题。烷化剂洛莫司汀可通过调节DNA损伤修复起到显著的抗白血病效应,那么在传统化疗中联合洛莫司汀治疗是否改善预后?近日,JCO杂志发表了LAM-SA 2007临床试验最新结果。
背景
急性髓系白血病(AML)的疾病发生率随年龄增长呈递增趋势,中位确诊年龄为70岁,预后很差,中位总生存期(OS)不足1年。洛莫司汀是一种烷化剂,通过调节DNA损伤修复起到显著的抗白血病效应。早期随机试验已显示洛莫司汀有改善临床预后的趋势,法国的一项回顾性研究亦证实了洛莫司汀在非高危细胞遗传学风险的老年AML患者中的潜在疗效。为改善这部分患者的预后,该开放性3期LAM-SA 2007临床试验评估了诱导化疗或巩固化疗联合洛莫司汀在老年非高危细胞遗传学风险AML患者中的预后价值。
方法
自2008年2月至2011年12月,该研究纳入了来自法国32个中心的459例年龄60-65岁老年AML患者(除急性早幼粒细胞白血病和孤立性粒细胞肉瘤之外),入组患者被随机分配至联合或不联合洛莫司汀的诱导化疗和巩固治疗组。诱导治疗方案为伊达比星8 mg/m2/d IV d1-5,阿糖胞苷100 mg/m2/d IV d1-7,联合(ICL)或不联合(IC)洛莫司汀200mg/m2 po d1。1个诱导化疗疗程后未获CR或CRi的患者不再接受二次诱导化疗,获得CR或CRi的患者则继续接受巩固治疗,方案为伊达比星8 mg/m2/d IV d1-3,阿糖胞苷50mg/m2 q12h IV d1-5,联合(ICL)或不联合(IC)洛莫司汀80mg po d1,1个巩固疗程后继续进行6个疗程的减量再诱导治疗,方案为:伊达比星8 mg/m2/d IV d1,阿糖胞苷50mg/m2 q12h IV d1-5,联合或不联合洛莫司汀40mg po d1。随后是包括6-巯嘌呤和甲氨蝶呤在内的6个月维持治疗。研究设计的具体流程见Figure1。本研究的主要目标为2年OS,次要目标为反应率,2年无事件生存率(EFS)和安全性。同时,本研究亦评估了累计复发率(CIR)和药物毒性所致的死亡率。

Figure 1
结果
2008年2月至2011年12月,该研究共招募了459例患者,最终227例和232例患者被随机分至A组(联合洛莫司汀)和B组(不联合洛莫司汀),两组中分别有209例和215例纳入分析。经评估两组患者的临床特征大致平衡(Table 1),中位年龄均为68岁,多数患者的ECOG PS和Sorror评分较低,90%的患者为细胞遗传学中危组。286例患者筛查了FLT3、NPM1和CEBPA的突变状态。

在参与随机分配并纳入分析的424例患者中,338例患者获得了CR(n=322)或CRi(n=16)。A组和B组的CR率为分别为78.9%和73%,CRi率分别为5.7%和1.8%,可见A组的反应率较B组显著提高(84.7% vs 74.9%,P = 0.01) 。同样地,A组的诱导治疗失败率也显著低于B组(8% vs 21%,P=0.001)。
所有患者诱导治疗后的中位随访期为24月,其中末次随访存活患者的中位随访期为48月。研究数据表明,在诱导治疗期间洛莫司汀对OS无显著影响,却能显著提高诱导治疗后的2年生存率(Fig 2A) ,A组和B组的诱导后2年OS分别为56%和48% 。
获得CR或CRi的338例患者中共209例患者复发(A组99例,B组110例)。其中,A组的2年CIR (40.2%) 显著低于B组(60.3%;Fig 2B )。A组的2年EFS (41%) 较B组(26%; Fig 2C) 显著提高。
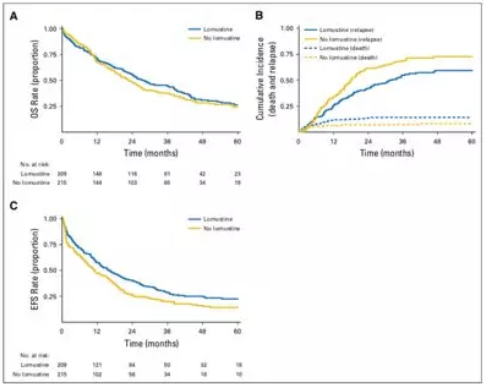
Figure 2
在血液学毒性评估上,A组在诱导和巩固治疗期间的毒性显著高于B组。而在诱导治疗期间的总体毒性评估上,A组亦显著高于B组(53% vs 40.9%) 。值得一提的是,两组由毒性导致的2年累计死亡率并无显著差异(12.4% vs 7.4%)。
讨论与总结
该研究旨在探讨在传统化疗联合洛莫司汀是否有助于提高非细胞遗传学高危老年AML患者的2年OS。尽管联合洛莫司汀组的早期死亡率更高(8% vs 4%),两者在诱导治疗期间的OS并无显著差异。然而,洛莫司汀组诱导后治疗的OS则显著提高(p=0.04),达成了该研究的主要目标。同时,1个诱导疗程后EFS、复发率、CR和CRi等次要目标指标在洛莫司汀组亦可见显著提高。因此,综合以上洛莫司汀带来的临床疗效,此药物可被考虑更为广泛地应用于老年AML患者。
原始出处:
Arnaud Pigneux, et al. Improved Survival by Adding Lomustine to Conventional Chemotherapy for Elderly Patients With AML Without Unfavorable Cytogenetics: Results of the LAM-SA 2007 FILO Trial. Journal of Clinical Oncology. Nov 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JCO#
58
#LAM#
71
谢谢分享学习
102
#结果公布#
0
#联合化疗#
56