J Thorac Oncol: 替雷利珠单抗(Tislelizumab)联合化疗一线治疗局部进展或转移性非鳞状非小细胞肺癌(nsq-NSCLC)的疗效和安全性(RATIONALE 304): 3期临床研究
2021-06-23 yd2015 MedSci原创
替雷利珠单抗(Tislelizumab)联合化疗一线治疗可以改善非鳞状非小细胞肺癌(nsq-NSCLC)患者的预后。因此其可以作为一线治疗的新选择。
非鳞状非小细胞肺癌(nsq-NSCLC)是非小细胞肺癌(NSCLC)常见的一种亚型。目前晚期nsq-NSCLC常用的一线治疗为免疫治疗联合化疗。目前批准用于治疗的免疫治疗有PD-1抑制剂(帕博利珠单抗和纳武利尤单抗)以及PD-L1抑制剂(阿替利珠单抗)等。但是,因为药物可及性,我国很多nsq-NSCLC患者并不能选择免疫治疗联合化疗。替雷利珠单抗(Tislelizumab)是一种国产的PD1抑制剂,已有2期临床研究数据证实替雷利珠单抗在多种晚期实体瘤中有抗肿瘤效果,包括非小细胞肺癌。同时,3期临床研究证实替雷利珠单抗(Tislelizumab)联合化疗可以改善晚期鳞状非小细胞肺癌患者的预后。近期,Journal of Thoracic Oncology发表了一项3期临床研究RATIONALE 304(NCT03663205),评估替雷利珠单抗(Tislelizumab)联合化疗一线治疗晚期非鳞状非小细胞肺癌(nsq-NSCLC)患者的疗效和安全性。

RATIONALE 304是我国上海胸科医院陆舜教授带头开展的一项开放标签、随机、多中心的3期临床研究,纳入病理确诊的 IIIB/IV nsq-NSCLC患者,随机2:1分配至联合治疗组(A):替雷利珠单抗(Tislelizumab)联合铂类 (卡铂或顺铂)+培美曲塞Q3W;化疗对照组(B):铂类 (卡铂或顺铂)+培美曲塞 Q3W。主要研究终点为无进展生存(PFS),次要研究终点为临床应答和安全性。
332例患者接受治疗,其中联合治疗组为222例,化疗组为110例。中位随访时间为9.8个月。替雷利珠单抗治疗的中位时间为31.6周(range: 3.0-78.4),大多数患者(n=135; 60.8%)接受9或以上周期的替雷利珠单抗(9-12周期, n=73 [32.9%]; >12周期的, n=62 [27.9%])。
替雷利珠单抗联合化疗较化疗组明显改善PFS,两组的PFS分别为9.7和7.6个月(HR=0.645 [95% CI: 0.462, 0.902]; P=0.0044)。两组的12个月PFS率分别为31.3% (95% CI: 21.7, 41.4) 和16.7% (95% CI: 6.8, 30.5)。亚组分析也发现免疫联合组较单纯化疗组取得生存获益。
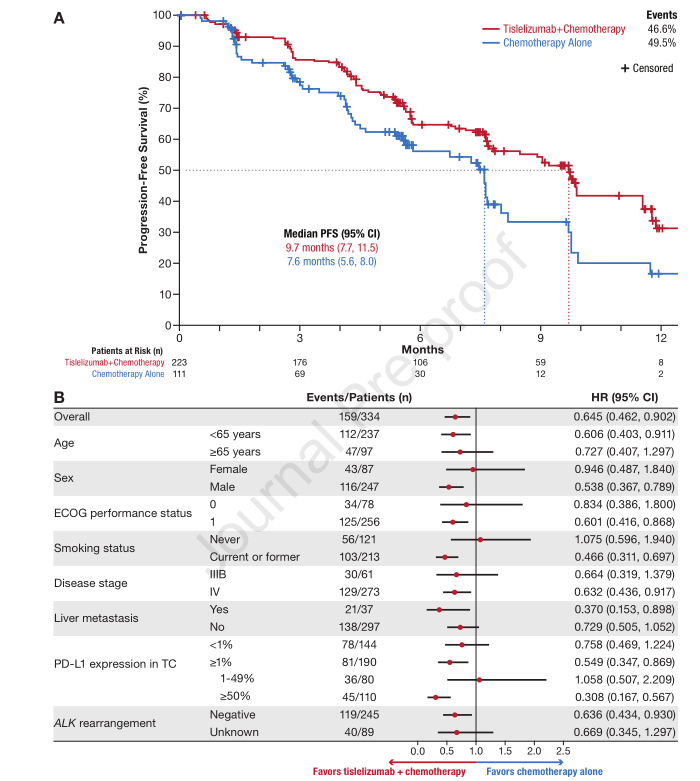
PFS和亚组分析
PD-L1 表达水平≥50%时,联合治疗组明显改善患者的PFS,为11.5和4.6个月。

PD-L1≥50%时PFS
免疫联合治疗组和单纯化疗组的客观缓解率(ORR)分别为57.4%(95% CI: 50.6-64.0) 和 36.9%(95% CI: 28.0-46.6)。中位持续缓解时间分别为8.5个月(95% CI:6.80, 10.58)和6.0个月 (95% CI: 4.99, 不可评估)。中位OS均未达到。

临床疗效
联合组中222例患者 (100%)以及化疗组中109例患者(99.1%)至少出现一种治疗相关不良事件(TEAE)。 两组常见的TEAE为血液学不良反应,大部分为1-2级。两组严重TEAEs分别为33.3%和20.9%。因为TEAEs导致治疗中断的比例分别为25.7%和9.1%。TEAEs导致替雷利珠单抗永久停用和剂量调整的比例分别为11.3%和59.9%。≥3级AEs包括中性粒细胞减少 (44.6% vs 35.5%), 白细胞减少(21.6% vs 14.5%), 血小板减少 (19.4% vs 13.6%), 和 贫血(13.5% vs 10.0%)。联合组和化疗组中分别有3例和1例患者因为TEAEs导致死亡。

治疗相关不良事件
综上,替雷利珠单抗(Tislelizumab)联合化疗一线治疗可以改善非鳞状非小细胞肺癌(nsq-NSCLC)患者的预后。因此其可以作为一线治疗的新选择。
原始出处:
Shun Lu, Jie Wang, Yan Yu, et al. Tislelizumab Plus Chemotherapy as First-line Treatment for Locally Advanced or Metastatic Nonsquamous Non-Small Cell Lung Cancer (RATIONALE 304): A Randomized Phase 3 Trial. J Thorac Oncol. 2021 May 22;S1556-0864(21)02176-6. doi: 10.1016/j.jtho.2021.05.005.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#THORAC#
62
#mAb#
73
#3期临床#
58
#Oncol#
67
#ratio#
72
#疗效和安全性#
71
#非小细胞#
0
#联合化疗#
56
#转移性非鳞状非小细胞肺癌#
57
#局部#
58