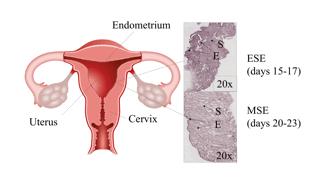
Hum Reprod:大数据揭示子宫内膜成熟新机制,或改善未来不孕不育的治疗
2018-10-14 风铃 生物探索
这项研究以“Endometrial receptivity revisited: endometrial transcriptome adjusted for tissue cellular heterogeneity”为题发表在生殖医学领域的权威期刊《Human Reproduction》上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#内膜#
57
学习了
94
学习了
93
#不孕不育#
67
#PRO#
45