Oncotarget:TUG1或是一个有潜力的胆管癌预后相关因素和治疗靶点
2017-08-08 Emma MedSci原创
胆管癌(CCA)是指源于肝外胆管包括肝门区至胆总管下端的胆管的恶性肿瘤,其病因可能与胆管结石、原发性硬化性胆管炎等疾病有关。其对常规化学疗法或放射治疗的反应差,预后不良,胆管癌一直被认为属于放射线不敏感的肿瘤,对化学治疗也并不敏感,胆管癌较其他胃肠道肿瘤例如结肠癌化疗敏感性差。
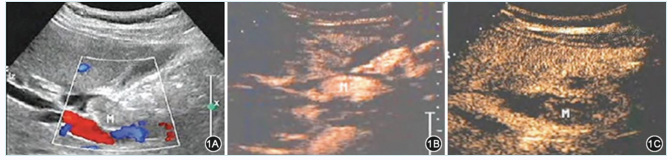
胆管癌(CCA)是指源于肝外胆管包括肝门区至胆总管下端的胆管的恶性肿瘤,其病因可能与胆管结石、原发性硬化性胆管炎等疾病有关。其对常规化学疗法或放射治疗的反应差,预后不良,胆管癌一直被认为属于放射线不敏感的肿瘤,对化学治疗也并不敏感,胆管癌较其他胃肠道肿瘤例如结肠癌化疗敏感性差。长非编码RNA(lncRNA)在多种人类癌症中起关键作用,有研究报道lncRNA牛磺酸上调基因1(TUG1)与人类癌症发展相关。发表于Oncotarget一篇文章中,研究人员调查了TUG1对CCA的影响,探讨TUG1的表达模式,并评估其临床意义以及对于CCA的预后潜力。研究结果表明,TUG1或是一个有潜力的CCA预后相关因素和治疗靶点。研究人员调查了TUG1的一系列功能作用,包括细胞增殖、凋亡、迁移、侵袭和上皮-间质转化(EMT)。数据显示,CCA组织和细胞系中TUG1上调,TUG1的过表达与CCA患者的肿瘤大小(p=0.005),TNM期(p=0.013),术后复发(p=0.036)和总生存期(p=0.010)有关。RNA沉默后TUG1下调,减少了CCA细胞的生长并且增加了CCA细胞的凋亡。此外,TUG1抑制能
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TUG1#
57
#治疗靶点#
54
#target#
58
#相关因素#
49
#胆管#
64
学习了新知识
91