JCO:3期| 吉非替尼 vs 顺铂+长春瑞滨辅助治疗手术切除后的非小细胞肺癌的预后
2021-11-04 Nebula MedSci原创
吉非替尼辅助治疗可防止非小细胞肺癌早期复发,但并不能延长无病生存期或总生存期
虽然以顺铂为基础的辅助化疗是手术完全切除的II期和III期非小细胞肺癌(NSCLC)的标准疗法,但患者的生存预后并不令人满意。一项对4584位患者进行的荟萃分析显示,以顺铂为基础的化疗与单纯观察作为术后辅助治疗的患者相比,仅显示了些许的临床益处。
本研究(IMPACT)旨在调查吉非替尼辅助治疗EGFR突变的非小细胞肺癌患者的疗效。
这是一项开放标签的随机的3期试验,招募了经手术完全切除的洗的EGFR突变(19号外显子缺失或L858R突变)的II-III期非小细胞肺癌患者,随机分成两组,接受吉非替尼(250 mg/日)治疗24个月或顺铂(80 mg/m2,第1天)联合长春瑞滨(25 mg/m2,第1和8天)治疗4个疗程(3周一疗程)。主要终点是无病生存期(DFS)。
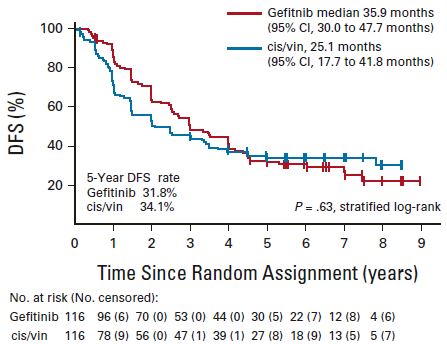
两治疗组的无病生存期
2011年9月至2015年期间,共招募了234位患者随机分至两组。在232位可评估患者(每组各116位)中,吉非替尼组和顺铂+长春瑞滨组的中位DFS分别是35.9个月和25.1个月。但是,Kaplan-Meier曲线在术后4年左右相交,无统计学差异(风险比 0.92,95% CI 0.67-1.28;p=0.63)。两组的总生存期(OS)也无显著差异(HR 1.03, 95% CI 0.65-1.65; p=0.89),5年OS率分别是78.0%个74.6%。顺铂+长春瑞滨组发生了3例治疗相关死亡,而吉非替尼组0例。
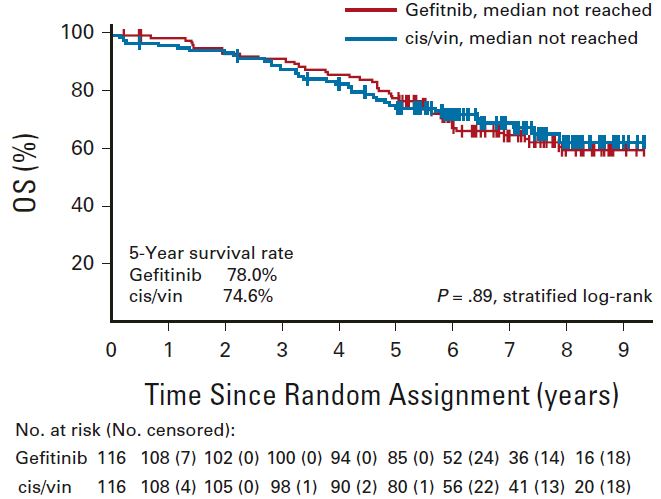
综上,虽然吉非替尼辅助治疗似乎可防止非小细胞肺癌早期复发,但并不能延长无病生存期或总生存期。但是,类似的DFS和OS可能证明在选定的患者亚群中使用吉非替尼辅助治疗是合理的,特别是那些被认为不适合铂双重辅助治疗的患者。
原始出处:
Tada Hirohito,Mitsudomi Tetsuya,Misumi Toshihiro et al. EGFRRandomized Phase III Study of Gefitinib Versus Cisplatin Plus Vinorelbine for Patients With Resected Stage II-IIIA Non-Small-Cell Lung Cancer With Mutation (IMPACT).[J] .J Clin Oncol, 2021, undefined: JCO2101729. https://doi.org/10.1200/JCO.21.01729
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#铂#
72
#JCO#
76
#非小细胞#
87
#手术切除#
89