JAHA:低循环肌素水平与经导管主动脉瓣植入术患者不良结局相关
2022-03-02 MedSci原创 MedSci原创
循环肌素是TAVI患者1年总生存率的独立预测因子。与EuroSCOREII相结合,循环肌素可能有助于提高对低至中等临床风险接受TAVI的患者死亡的预测水平。
肌素是一种活动刺激和心脏保护性肌因子,可减轻病理性心脏重塑。反过来,肌素缺乏会导致身体耐力下降。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究的目的是评估循环肌素作为一种新的、推定的生物标志物的预后价值,以识别死亡风险较高的经导管主动脉瓣植入术(TAVI)患者。

在这项研究中,研究人员测量了368名接受TAVI的患者的全身肌素水平,这些患者的临床风险处于低到中度(中位数EuroSCORE[欧洲心脏手术风险评估系统]II为3.5;四分位数1-四分位数为2.2%-5.3%),其中209名(56.8%)患者处于低风险,159名(43.2%)处于中等风险。术前肌素中位数为2.7ng/mL(四分位数1-四分位数3为1.5-4.6ng/mL)。
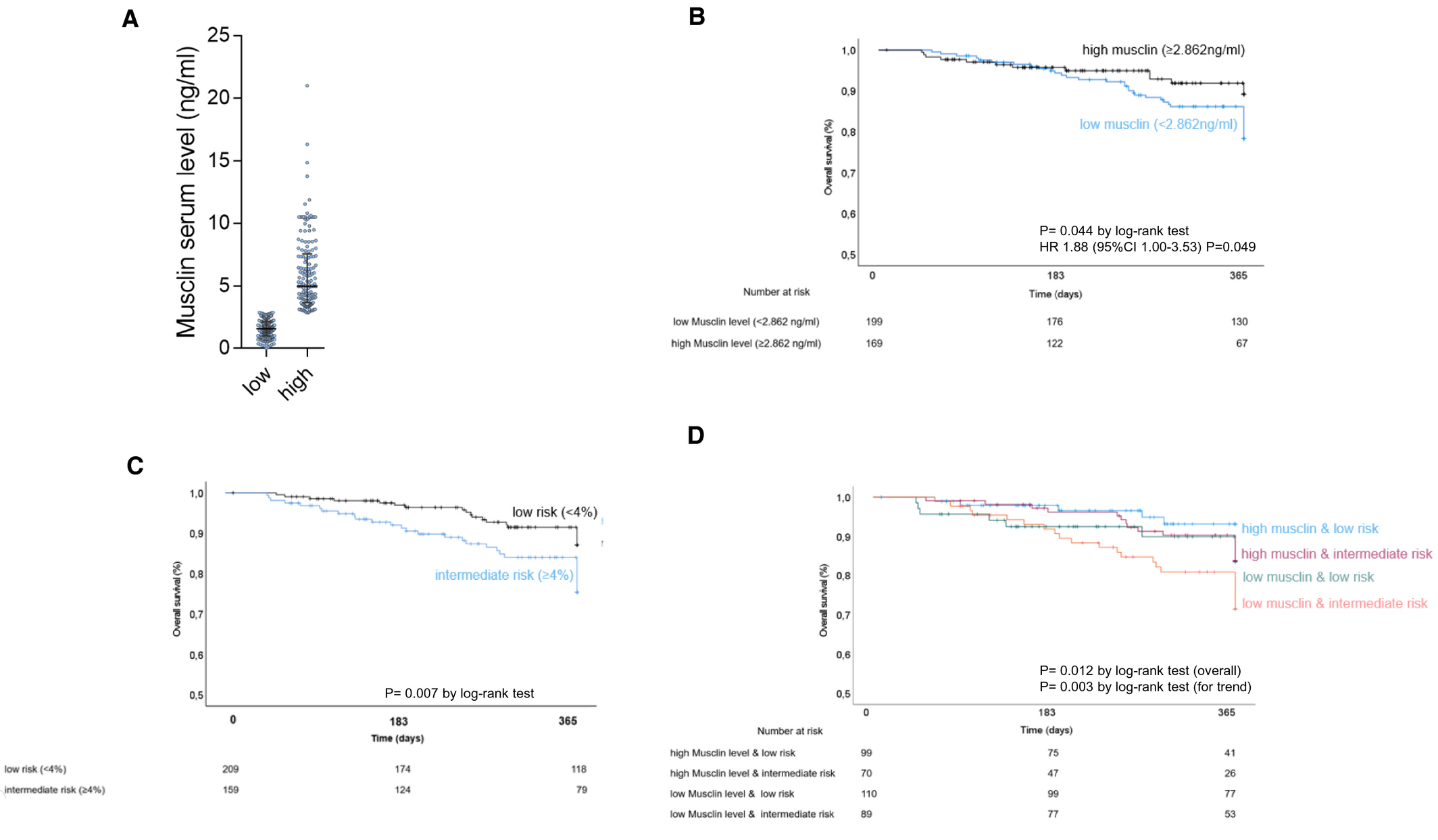
研究人员使用通过分类和回归树分析确定的临界值将肌肉素水平分为低水平组(<2.862ng/mL,n=199[54.1%])或高水平组(≥2.862ng/mL,n=169[45.9%])。该研究的主要终点是1年总生存期。循环肌素水平较低的患者虚弱、白蛋白值低、高血压和卒中病史以及较高的B型利钠肽前体N末端的患病率显著升高。在Cox回归分析中,低肌素水平显著预测单变量(风险比为1.81;95%CI为1.00-3.53[P=0.049])和多变量(调整后的风险比为2.45;95%CI为1.06-5.69[P=0.037])的死亡风险。此外,低肌素水平与传统EuroSCOREII相结合表明,通过时序检验将低至中度临床风险接受TAVI的患者分为1年生存率降低的亚组的风险分层得到了改善(趋势P=0.003)。
由此可见,循环肌素是TAVI患者1年总生存率的独立预测因子。与EuroSCOREII相结合,循环肌素可能有助于提高对低至中等临床风险接受TAVI的患者死亡的预测水平。
原始出处:
Badder Kattih.et al.Low Circulating Musclin is Associated With Adverse Prognosis in Patients Undergoing Transcatheter Aortic Valve Implantation at Low‐Intermediate Risk.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.022792
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#经导管主动脉瓣植入#
85
#主动脉瓣植入术#
72
#AHA#
78
#主动脉瓣#
71
#主动脉#
79
#经导管#
80
#植入#
96