JGABSMS:健康的行为、休闲活动和社交网络延长老年糖尿病患者的无残疾生存期
2022-03-19 从医路漫漫 MedSci原创
2型糖尿病(T2 DM)影响着全球1.356亿 65岁的人,这一数字预计到2045年将达到2.762亿。2型糖尿病与更高的残疾风险和过度死亡率有关,这对我们的社会造成了相当大的经济影响。

背景:2型糖尿病(T2DM)影响着全球1.356亿≥65岁的人,这一数字预计到2045年将达到2.762亿。2型糖尿病与更高的残疾风险和过度死亡率有关,这对我们的社会造成了相当大的经济影响。鉴于人口老龄化和T2 DM的高患病率,确定预防这些不良健康后果的策略,并延长患有T2 DM的老年患者的独立生存已成为公共卫生的优先事项。
越来越多的证据表明,糖尿病与残疾风险增加1.5-1.8倍,过度死亡风险增加1.1-1.9倍,这取决于年龄、血糖控制和并发症的存在。一些流行病学研究表明,健康的生活方式,包括单独和共同的行为(如饮酒和吸烟)和休闲活动,对T2 DM患者的健康结果有好处。此外,拥有中等到丰富的社交网络与身体功能受损、残疾和死亡率呈负相关。由于丰富的社会网络可以降低患T2 DM的风险,可以预期社会网络对继发于T2 DM的长期结果的有利影响。然而,关于社交网络与T2 DM患者的不良健康后果之间的关联的证据很少。
尽管生活方式因素已单独与T2 DM及其并发症相关,但多种生活方式因素的联合作用仍不确定。由于这些生活方式因素往往聚集在一起,它们对健康的协同作用可能比单独因素的影响更大。然而,生活方式特征在多大程度上可以帮助患有T2 DM的老年人在没有依赖的情况下活得更长,目前还不清楚。我们此前曾报道,参与休闲活动和中等至丰富的社交网络可能会降低T2 DM患者患痴呆症的风险。在本研究中,我们的目标是1)估计T2 DM缩短无残疾生存期的程度,2)探索健康的生活方式(包括健康的行为、积极的休闲活动和中等至丰富的社会网络)是否以及在多大程度上可以延长患有T2 DM的老年患者的无残疾生存期。
目的:糖尿病与残疾和超额死亡率有关。我们估计了糖尿病缩短无残疾生存期的程度,并确定了可能延长老年糖尿病患者无残疾生存期的可修改因素。
方法:对2216名无残疾老年人(平均年龄:71岁,女性:61%)进行长达15年的随访。糖尿病是通过医疗检查、药物使用或糖化血红蛋白≥6.5%(48 mmoL/摩尔)来确定的。无残疾生存被定义为直到残疾发生的生存。有利(与不利)的生活方式被定义为至少存在以下一种情况:健康(与不健康的)行为,积极(与不积极)参与休闲活动,或中等至富裕(与贫穷)的社交网络。数据分析采用COX回归和Laplace回归。
结果:在随访期间,1,345名参与者(60.7%)出现残疾或死亡。糖尿病,而不是糖尿病前期,与结果相关(风险比[HR]1.29,95%可信区间1.06-1.57),以及2.15年(1.02-3.27)年的中位无残疾生存期缩短。在联合暴露分析中,患有糖尿病并有不健康行为、不积极参与休闲活动或社交网络较差的参与者的无残疾生存期缩短了3.29年(1.21-5.36)、3.92年(2.08-5.76)和1.66年(0.06-3.28)。在患有糖尿病的参与者中,良好的特征导致非显著的残疾/死亡比率为1.19(0.93-1.56),与特征不佳的参与者相比,无残疾生存期延长3.26(2.33-4.18)年。
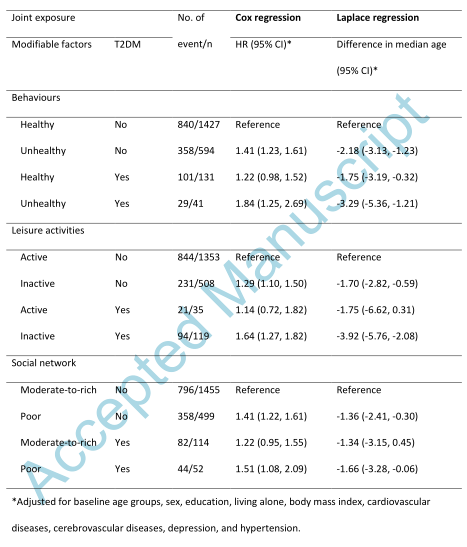
表1 危险比(HR),95%可信区间(CI),以及生活方式因素、休闲活动和社会网络加T2 DM对事件综合结果的中位数差异。
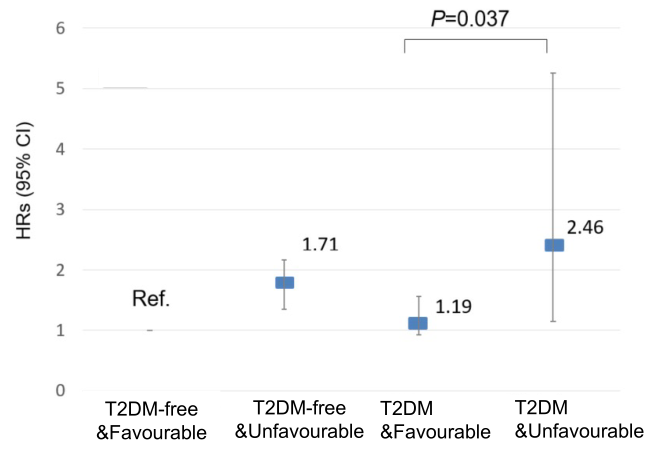
图1 健康行为、积极的休闲活动和中等到丰富的社会网络对残疾/死亡风险的联合关联(根据对基线年龄组、性别、教育程度、生活状况、体重指数、心血管疾病、脑血管疾病、抑郁症和高血压进行调整的Cox回归模型进行调整)。“良好形象”指的是至少有一种健康的行为、积极参与休闲活动或中等至富裕的社交网络。“不良形象”指的是没有任何健康的行为,没有积极参与休闲活动,或者没有中等到丰富的社交网络。HR:危险比;CI:可信区间p=0.037是指“T2 DM+有利”组与“T2 DM+不利”组复合终点风险差异的显著水平。
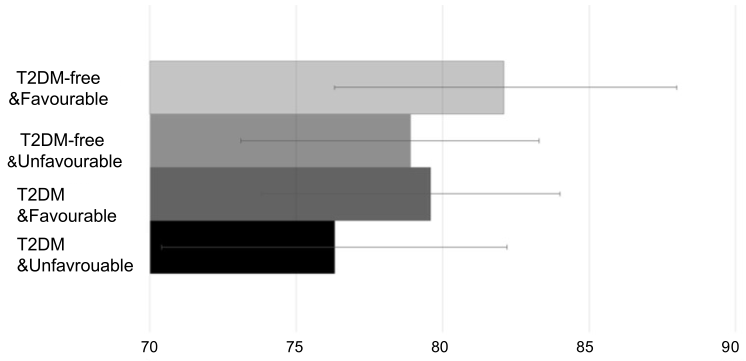
图2 根据T2 DM状况和良好状况的残疾或死亡年龄中位数。通过拟合多变量拉普拉斯回归模型,对基线年龄组、性别、教育程度、生活状况、体重指数、心血管疾病、脑血管疾病、抑郁症和高血压进行调整,获得估计值。“良好形象”指的是至少有一种健康的行为、积极参与休闲活动或中等至富裕的社交网络。“不良形象”指的是不具备健康的生活方式、积极的休闲活动或中等至富裕的社交网络等因素。
结论:健康和积极的社交生活方式可能会降低糖尿病致残或死亡的风险,并延长糖尿病患者的无残疾生存期。
原文出处: Shang Y, Wu W, Dove A, et al.Healthy behaviours, leisure activities, and social network prolong disability-free survival in older adults with diabetes.J Gerontol A Biol Sci Med Sci 2022 Mar 03
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#社交网络#
88
#生存期#
85
#糖尿病患者#
86
#老年糖尿病#
93
#社交#
74