无论是在全球还是在中国,肺癌都是发病率最高的恶性肿瘤,且是导致癌症死亡的主要原因,其中非小细胞肺癌(NSCLC)约占肺癌总数的80%~85%。据国家癌症中心最新统计数据,我国2015年新增约78.7万肺癌患者,约63.1万人因肺癌死亡。
根据《原发性肺癌诊疗规范(2018年版)》,我国NSCLC患者中,晚期患者五年生存率仅为5%左右,治疗现状亟需改善。
去年北美肺癌大会上,pembrolizumab(Keytruda,简称K药)联合化疗(卡铂+培美曲塞)一线治疗晚期NSCLC的长期生存数据公布:超过一半患者存活超过了3年,相较于化疗,死亡风险显著降低29%,为广大NSCLC患者带来了希望。
手术切除仍然是早期NSCLC管理的标准治疗方法。鉴于延迟的手术治疗在理论上具有疾病进展的风险,因此预后不佳,NSCLC患者应及时接受治疗。但目前,有关肺癌诊断和手术治疗或一般的治疗之间是否存在一个安全期,目前还不清楚。
鉴于先前的研究对癌症诊断日期使用了不精确的定义,人们对NSCLC患者的延迟手术治疗和肿瘤学结果之间的关系了解甚少。来自美国华盛顿医学院手术中心的专家使用一个统一的方法来量化手术治疗延迟,并检查其与几种肿瘤学结果的关系,相关结果发表在《美国医学会杂志》子刊JAMA Network Open杂志上。
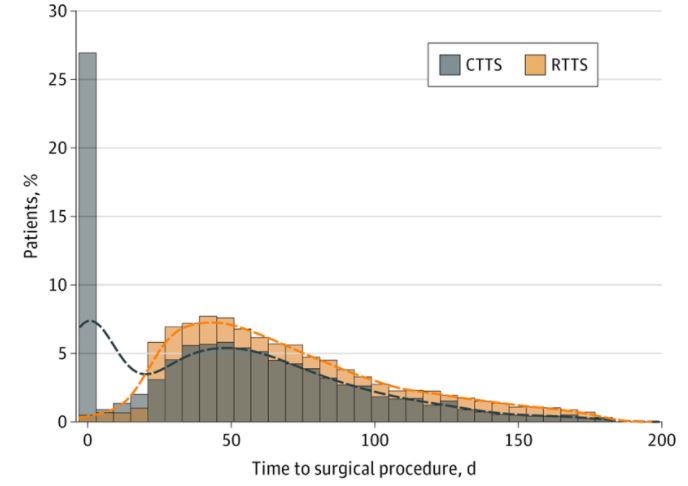
这项回顾性队列研究是利用退伍军人健康管理局(VHA)系统的一个新数据集进行的。纳入的患者为临床I期NSCLC,2006年至2016年在VHA系统内接受切除手术。主要的暴露因素为等待癌症诊断和手术治疗之间的时间(即TTS,术前诊断性计算机断层成像和手术治疗之间的时间)。
通过临床或放射学方法对延迟的手术治疗进行量化
在9904名接受手术治疗的临床I期NSCLC患者中,9539人(96.3%)为男性,4972人(50.5%)目前吸烟,平均(SD)年龄为67.7(7.9)岁。平均TTS为70.1天。TTS与病理分期或阳性边缘的风险增加没有关系。4158名患者(42.0%)检测到复发,随访时间中位数为6.15年。
总的来说,与复发风险增加相关的因素包括年龄较小(每年轻1岁,风险增加8%),较高的Charlson并发症指数评分(每增加1个单位,风险增加5.5%),分段切除(与肺切除术相比,风险增加35.2%)或楔形切除(与肺切除术相比,风险增加28.2%),更大的肿瘤尺寸、更高的肿瘤等级、较少的淋巴结检查、较高的病理分期以及较长的TTS。
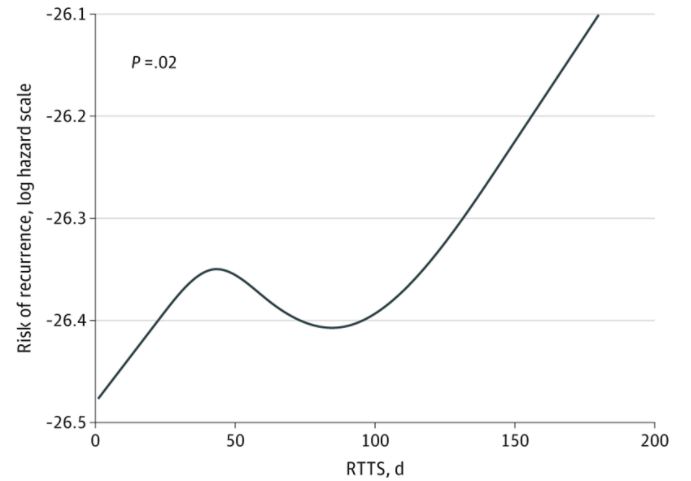
放射性手术治疗时间(RTTS)与复发概率之间的关系
超过12周后,手术每推迟一周,复发的危险就增加0.4%。与延迟手术治疗相关的因素包括非裔美国人、较高的地区贫困指数[ADI]得分、较低的医院病例数。在诊断后12周内进行手术治疗的患者的总生存率明显高于手术延迟超过12周的患者(HR=1.132;95%CI,1.064-1.204)。
综上,这项研究发现,延迟12周以上的外科手术与复发风险增加和生存率降低有关。这些发现表明,临床I期NSCLC患者应在该时间范围内接受快速治疗。
参考文献:
Heiden BT, Eaton DB, Engelhardt KE, et al. Analysis of Delayed Surgical Treatment and Oncologic Outcomes in Clinical Stage I Non–Small Cell Lung Cancer. JAMA Netw Open. 2021;4(5):e2111613. doi:10.1001/jamanetworkopen.2021.11613
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#细胞癌#
71
#复发风险#
61
#小细胞癌#
68
#非小细胞#
46
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
98
挺好的文章
67