JAMA:持续高渗液体治疗对创伤性脑损伤患者神经功能改善无益
2021-05-26 MedSci原创 MedSci原创
在中重度创伤性脑损伤患者中,持续输注20%高渗盐水治疗与标准治疗相比,在6个月时神经功能改善方面无显著差异,持续输注高渗盐水正在改善TBI患者临床功能方法的作用有限
据估计,2019年全球6900万人经历了各种原因的创伤性脑损伤(TBI)。在过去几十年里,TBI后患者死亡率稳步下降,但致残率仍很高,2016年TBI后严重残疾患者高达800多万。液体疗法是预防和治疗继发性脑损伤的主要组成部分。有研究称,持续血液高渗可预防或治疗TBI创伤后颅内高压,提高生存率,但由于长期临床数据有限,神经重症监护指南不推荐连续预防性高渗复苏液治疗。近日研究人员考察了持续注射高渗生理盐水对创伤性脑损伤患者6个月神经预后的影响。
COBI研究在法国9个重症监护中心开展,370名中重度颅脑损伤患者参与,在标准护理基础上,随机接受连续输注20%高渗盐水(n=185)或对照(对照组,n=185)。若患者有持续颅内高压风险,则至少给予48小时的20%高渗盐水治疗。研究的主要终点为6个月时扩展格拉斯哥结局量表评分(GOS-E,范围为1-8,评分越低,功能结果越差),次要结果总计12个,包括颅内高压和6个月死亡率。
患者平均年龄44岁,77名(20.2%)女性,359名(97%)患者完成了试验。6个月时,组间GOS-E评分的校正比值比(OR)为1.02。在12个次要结果中,10个无显著差异,但高渗盐水干预组颅内高压(62例vs 66例,33.7% vs 36.3%,绝对差异为-2.6%,OR=0.80)和6个月死亡风险(29例vs 37例,15.9% vs 20.8%,绝对差异为-4.9%,HR=0.79)略低,但差异不显著。
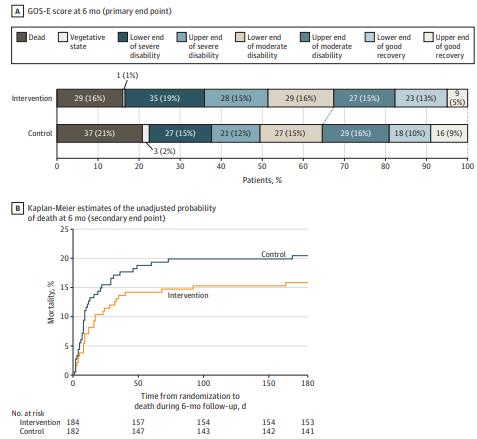
组间神经功能改善与死亡风险评估
在中重度创伤性脑损伤患者中,持续输注20%高渗盐水治疗与标准治疗相比,在6个月时神经功能改善方面无显著差异,持续输注高渗盐水正在改善TBI患者临床功能方法的作用有限。
原始出处
Antoine Roquilly et al. Effect of Continuous Infusion of Hypertonic Saline vs Standard Care on 6-Month Neurological Outcomes in Patients With Traumatic Brain Injury The COBI Randomized Clinical Trial.JAMA. May 25, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#创伤性#
82
学习了
95
学习了
96
#创伤#
78
#损伤#
78
#神经功能#
91
#液体治疗#
74
好
116
学到了
106
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
80