Oncogene:新蛋白质可以预测乳腺癌肺转移
2012-04-10 Beyond 生物谷
最近,研究人员发现一种有用蛋白质,该蛋白质可以预测乳腺癌患者发生肺转移的风险 过氧化物酶2保护肿瘤细胞免受氧化应激,并促进肿瘤细胞在肺部的生长和增殖。 来自Bellvitge生物医学研究所(IDIBELL)的研究表明:转移到肺的乳腺癌细胞能表达较高水平的过氧化物酶2(PRDX2)蛋白。这项研究证实调控这种蛋白质的水平可能是一个新的治疗肿瘤,以防止肺转移的策略。研究结果发表在Oncogene杂志
最近,研究人员发现一种有用蛋白质,该蛋白质可以预测乳腺癌患者发生肺转移的风险
过氧化物酶2保护肿瘤细胞免受氧化应激,并促进肿瘤细胞在肺部的生长和增殖。
来自Bellvitge生物医学研究所(IDIBELL)的研究表明:转移到肺的乳腺癌细胞能表达较高水平的过氧化物酶2(PRDX2)蛋白。这项研究证实调控这种蛋白质的水平可能是一个新的治疗肿瘤,以防止肺转移的策略。研究结果发表在Oncogene杂志上。
PRDX2是一个氧化还原酶,能保护细胞免受自由基和氧化应激的损伤。PRDX2对肺部肿瘤细胞能生活在充足氧气的环境中至关重要。在乳腺癌细胞中,过度表达的PRDX2可防止氧化应激的损伤,促进肺部肿瘤的生长、增殖和转移。
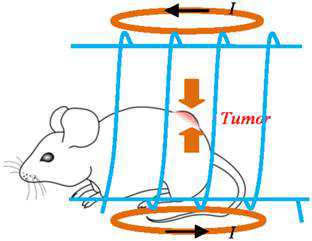
Sierra等研究者用细胞实验以及小鼠动物模型证实了低表达水平的PRDX2足以阻止转移性肿瘤细胞转移至肺。
Sierra说:“这些研究结果表明修改的PRDX2表达可能会产生一种新的治疗方法,以防止肿瘤细胞肺转移,一些抑制该蛋白的药物的有效性已经在其他疾病中得到测试。
下一步研究工作就是能得到足够数量的高表达这种蛋白的患者,验证PRDX2能否作为乳腺癌肺转移风险的生物标志物。(生物谷:Bioon)

doi:10.1038/onc.2012.93
PMC:
PMID:
Peroxiredoxin 2 specifically regulates the oxidative and metabolic stress response of human metastatic breast cancer cells in lungs.
Stresing V, Baltziskueta E, Rubio N, Blanco J, Arriba M, Valls J, Janier M, Clézardin P, Sanz-Pamplona R, Nieva C, Marro M, Dmitri P, Sierra A.
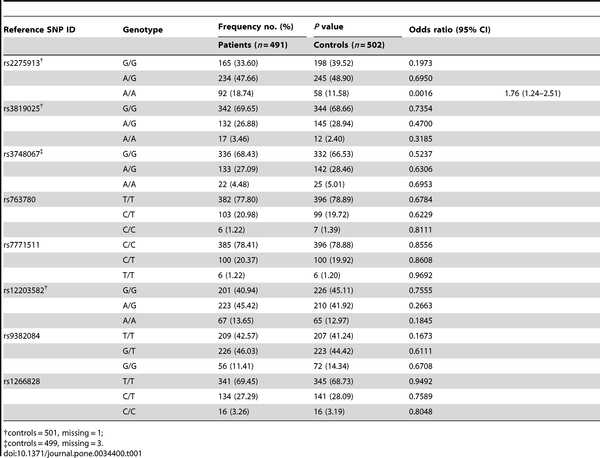
Little is known about metastatic pathways that are specific to the lung rather than other organs. We previously showed that antioxidant proteins such as peroxiredoxins were specifically upregulated in lung metastatic breast cancer cells. We hypothesize that cancer cells that live under aerobic conditions, as might be the case in lungs, protect themselves against the damage caused by reactive oxygen species (ROS). To examine this hypothesis, we studied the role of peroxiredoxin-2 (PRDX2) in lung vs bone metastasis formation. A metastatic variant of MDA-MB-435 breast cancer cells that specifically metastasize to lungs (435-L3) was transduced with short hairpin RNAs to specifically silence PRDX2. Conversely, a bone metastatic variant of MDA-MB-231 cells (BO2) was stably transfected to overexpress PRDX2. The 435-L3 cells silenced for PRDX2 were significantly more sensitive to H(2)O(2)-induced oxidative stress than the parental and scrambled transfected cells. BO2/PRDX2 cells produced less ROS than BO2/green fluorescent protein control cells under oxidative stress. Moreover, PRDX2 knockdown inhibited the growth of 435-L3 cells in the lungs, whereas lymph node metastasis remained unaffected. In contrast, PRDX2 overexpression in bone metastatic BO2 breast cancer cells led to drastic inhibition of the skeletal tumor burden and reduction of bone destruction. Furthermore, PRDX2 expression in breast cancer cells was associated with a glucose-dependent phenotype, different from bone metastatic cells. Overall, our results strongly suggest that PRDX2 is a targetable 'metabolic adaptor' driver protein implicated in the selective growth of metastatic cells in the lungs by protecting them against oxidative stress.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#白质#
60
#Gene#
65
#蛋白质#
85
#肺转移#
72
#Oncogene#
79