CheckMate-078研究:首次印证免疫治疗在中国人群的疗效和安全性
2018-07-13 佚名 肿瘤资讯
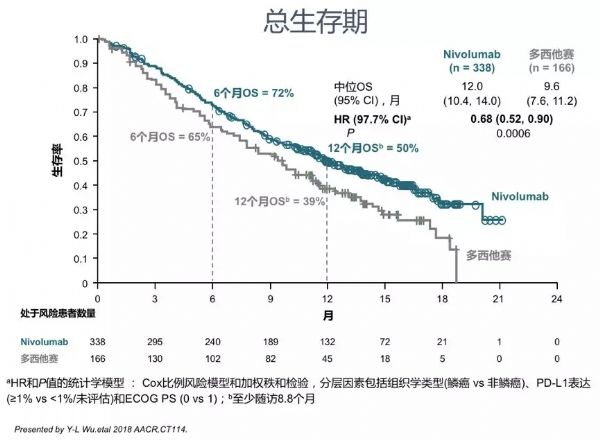
CheckMate-078研究是第一项针对东亚人群,特别以中国人群为主的免疫检查点抑制剂二线治疗晚期NSCLC的临床研究。与纳武利尤单抗(Nivolumab)在全球注册临床CheckMate-017研究和CheckMate-057研究结果一致,在CheckMate-078研究中,纳武利尤单抗对比化疗显著降低患者的死亡风险。该研究成功的进一步验证了纳武利尤单抗的卓越疗效和安全性。基于CheckMat
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Checkmate#
77
#疗效和安全性#
97
可以呀,学习学习
100
怎么收藏
143
谢谢梅斯提供这么好的信息,学到很多
88
好
123
谢谢分享学习了
97