JAMA Surg:氨甲环酸用于大手术出血风险的预防及安全性研究
2021-04-20 MedSci原创 MedSci原创
静脉注射氨甲环酸用于大手术出血风险的预防是安全的,不会导致血栓栓塞事件风险增加
大手术通常会导致患者大量失血,并导致随后贫血和输血需求风险增加。VISION研究称,在40004 名接受非心脏手术的患者中,最常见的导致死亡的并发症是大出血后心肌损伤和感染。氨甲环酸(TXA)是一种抗纤维蛋白溶解剂,广泛用于预防和治疗高纤维蛋白溶解引起的出血。Poeran等研究人员发现,TXA显著减少了大手术失血和相关并发症风险,2012年的临床使用率达11.2%。在众多TXA相关不良事件中,血管闭塞性事件是十分危险的。
近日研究人员考察了静脉注射氨甲环酸的总血栓栓塞事件(TEs)风险。

本次研究为系统综述及荟萃分析研究,收集1976-2020年间相关研究,比较静脉注射TXA或安慰剂治疗后的不良事件。研究的主要终点为血管闭塞事件和死亡率。
总计216个试验,包括125550名患者。TXA组总TEs发生1020例(2.1%),对照组有900例(2.0%)。研究发现静脉注射TXA与静脉血栓形成、肺栓塞、静脉TEs、心肌梗死或缺血、脑梗死或缺血风险(风险差异=0.001)之间没有关联。研究发现,使用TXA后,患者总死亡率和出血死亡率显著降低,但对非出血死亡率无显著影响。此外,在包含血栓病史的患者研究中,没有发现TXA对血管闭塞事件的影响。比较样本量小于或等于99(风险差异=0.004)、100至999(风险差异=0.004)和大于或等于1000(风险差异=-0.001)研究之间的结果差异,未发现样本量对TXA-总TEs风险的影响。TXA治疗剂量与静脉TEs风险无关(风险差异=-0.005)。
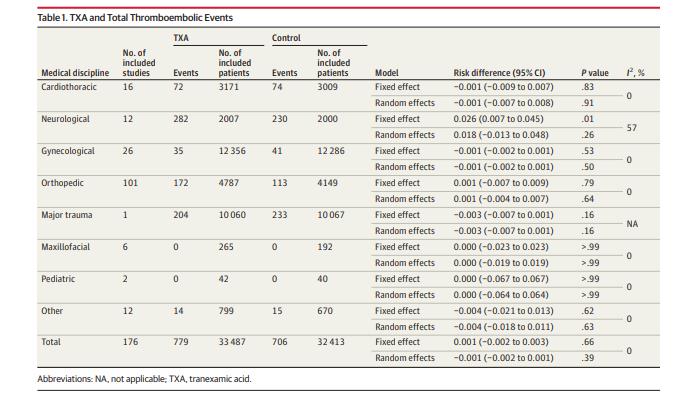
研究认为,静脉注射氨甲环酸用于大手术出血风险的预防是安全的,不会导致血栓栓塞事件风险增加。
原始出处:
Isabel Taeuber et al. Association of Intravenous Tranexamic Acid With Thromboembolic Events and Mortality A Systematic Review, Meta-analysis, and Meta-regression.JAMA Surg. April 14, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#大手术#
89
优秀
120
好
125
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
104
好
111