J Clin Oncol:震惊!局部晚期可切除的食管癌患者从术前放化疗中的生存获益可至少持续10年!
2021-04-26 Nebula MedSci原创
根据CROSS标准,局部晚期的可切除食管癌或交界癌患者从术前放化疗中获得的总体生存益处可至少持续10年!
食管癌是常见的消化道肿瘤,全世界每年约有30万人死于食管癌。其发病率和死亡率各国差异很大。我国是世界上食管癌高发地区之一,每年平均病死约15万人。男多于女,发病年龄多在40岁以上。食管癌典型的症状为进行性咽下困难,先是难咽干的食物,继而是半流质食物,最后水和唾液也不能咽下。

根据食管癌先放化疗后手术的原则,术前放化疗已成为局部晚期可切除食管癌或交界癌患者的标准治疗方案。本研究目标是评估这种疗法的长期预后。
从2004年到2008年,研究人员随机将366名患者分为两组,接受卡铂+紫杉醇(5周/疗程)联合放疗(每周5天,23次,共41.4Gy),然后手术,或单纯手术。随访数据收集到2018年。采用COX回归分析比较总体生存率、特定原因生存率以及局部复发和远处复发的风险。
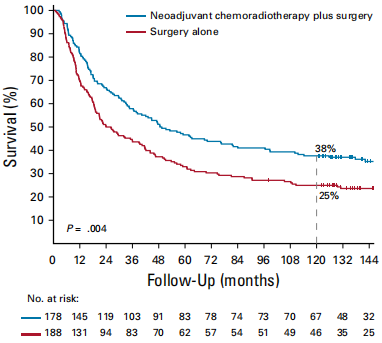
总存活率
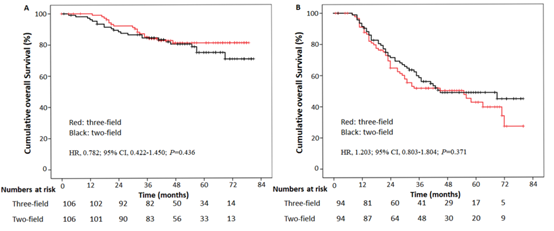
中位随访时间147个月(四分位数范围:134-157)。接受新辅助放化疗的患者的总体存活率较高(风险比[HR] 0.70;95%CI 0.55-0.89)。新辅助放化疗对总存活率的影响不依赖于时间(交互作用P值=0.73),里程碑式的分析表明,在长达10年的随访过程中,新辅助放化疗对总存活率的影响较为稳定。
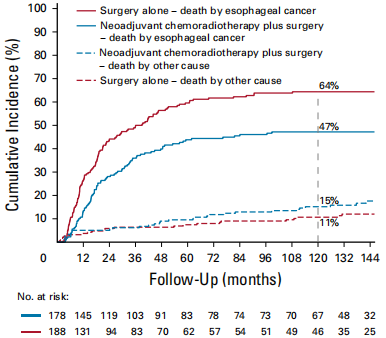
不同原因的累积死亡率
10年的绝对总体生存收益为13%(38% vs 25%)。新辅助放化疗明显降低了食管癌工作的死亡风险(HR 0.60;95%CI 0.46-0.80)。其他原因死亡在研究组之间相似(HR 1.17;95%CI 0.68-1.99)。
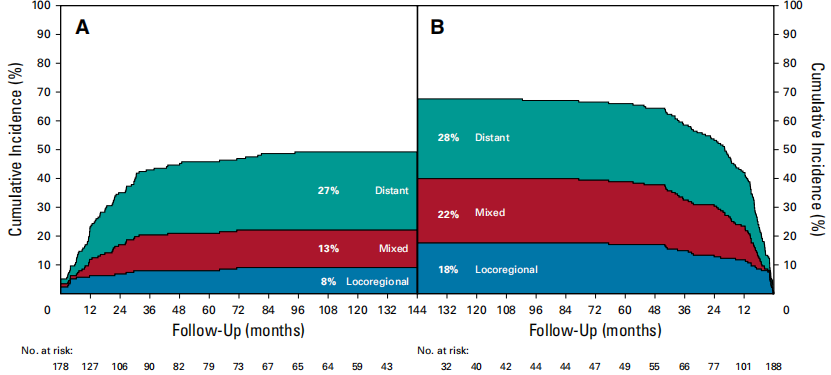
累积复发率
虽然对孤立性局部复发(HR 0.40;95%CI 0.21-0.72)和同步局部区域+远处复发风险(HR 0.43;95%CI 0.26-0.72)有明显影响,但孤立性远处复发也具有一定可比性(HR 0.76;95%CI 0.52-1.13)。
总之,根据CROSS标准,局部晚期的可切除食管癌或交界癌患者从术前放化疗中获得的总体生存益处可至少持续10年!
原始出处:
Eyck Ben M,van Lanschot J Jan B,Hulshof Maarten C C M et al. Ten-Year Outcome of Neoadjuvant Chemoradiotherapy Plus Surgery for Esophageal Cancer: The Randomized Controlled CROSS Trial. J Clin Oncol, 2021, undefined: JCO2003614. https://doi.org/10.1200/JCO.20.03614
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#食管癌患者#
102
#Oncol#
83
#生存获益#
96
#局部晚期#
69
#放化疗#
75
#局部#
75
#食管#
74
谢谢梅斯分享这么多精彩信息
89
获益10年
144