ARD:使用生物 DMARD的RA患者队列中急性冠状动脉综合征的短期、中期和长期风险:来自四个北欧国家的结果
2022-04-04 MedSci原创 MedSci原创
与一般人群相比,使用生物类疾病改善抗风湿药(bDMARDs)的类风湿性关节炎患者急性冠状动脉综合征(ACS)发生率较高。在常规护理中使用时,ACS 的短期、中期和长期风险在各bDMARD之间差别不大。
目的:类风湿性关节炎 (RA) 患者患急性冠状动脉综合征 (ACS) 和其他心血管疾病的风险增加,但在这些风险方面,不同的生物/靶向合成疾病缓解抗风湿药 (b/tsDMARD) 之间的比较尚不清楚,大多数研究都比较了一种b/tsDMARD与另一种的风险,而不是所有可用的b/tsDMARD之间的风险。本研究目的在于比较RA患者在开始使用目前临床实践中可用的任何生物类疾病改善抗风湿药(bDMARDs)的1年、2年和5年ACS发生率,并和一般人群进行比较。
方法:观察性队列研究,来自丹麦、芬兰、挪威和瑞典的患者在2008-2017年期间开始bDMARD治疗。通过注册链接确定第一次ACS的时间。研究者计算了1年、2年和5 年的发病率(IR)(药物治疗和治疗开始后),并使用Cox回归 (HRs) 比较了不同治疗的ACS发病率(考虑ACS风险因素)。在按年龄、既往bDMARD次数和心血管疾病史定义的亚组中进一步分别进行分析。研究者还将ACS发病率与单独匹配的一般人群队列进行了比较。
结果:共纳入40850个疗程的24083名患者(75%为女性,平均年龄56岁)。在最长(5 年)随访期间(141257人年(pyrs)),发生780起ACS事件(粗IR 5.5/1000 pyrs)。总体而言,RA中ACS的发生率比一般人群高80%。对于所有bDMARD和不同随访时间点,HR接近1(依那西普作为参考),但5年风险窗口除外,其中阿巴西普(ABA)、英夫利昔单抗(INF)和利妥昔单抗(RIT)的HR值大于1。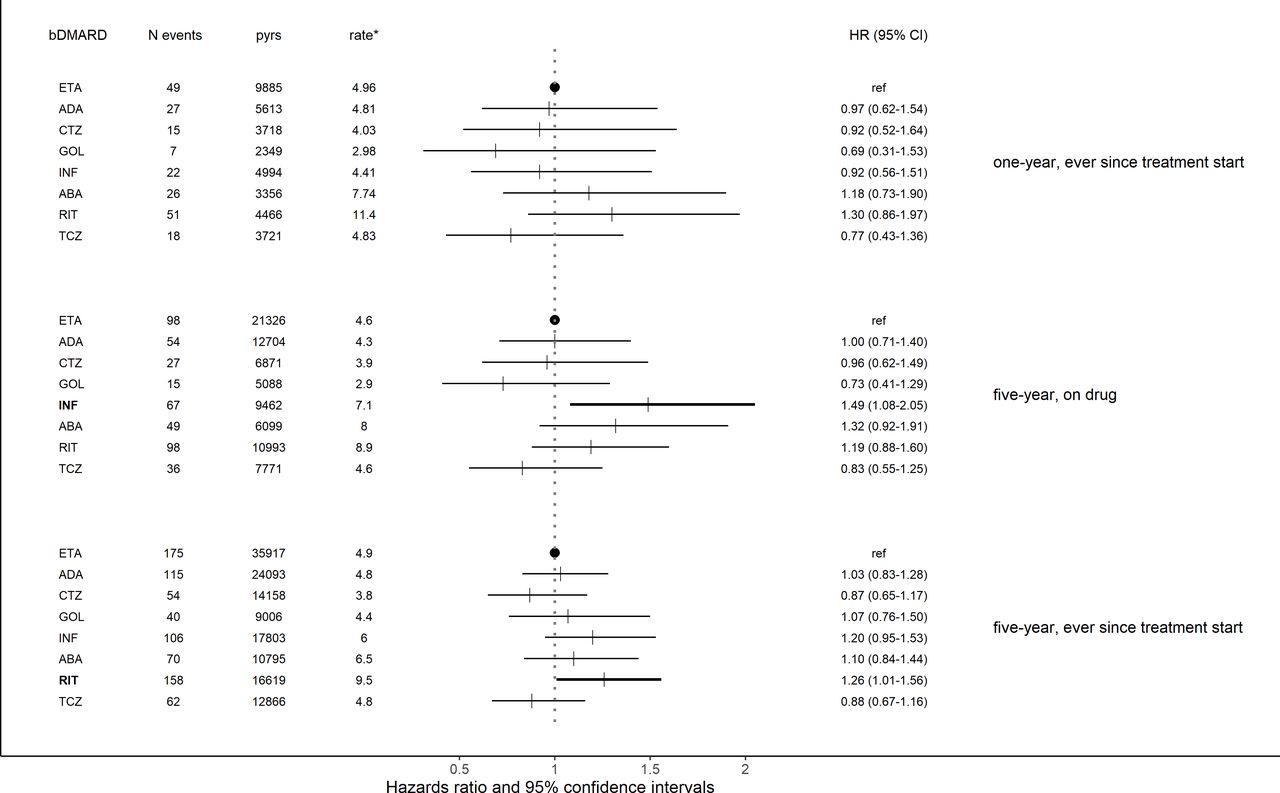
结论:与一般人群相比,使用bDMARDs的RA患者ACS发生率较高。在常规护理中使用时,ACS 的短期、中期和长期风险在各bDMARD之间差别不大。
出处:Delcoigne B, Ljung L, Provan SA, et al. Short-term, intermediate-term and long-term risks of acute coronary syndrome in cohorts of patients with RA starting biologic DMARDs: results from four Nordic countries. Annals of the Rheumatic Diseases. Published Online First: 22 March 2022. doi: 10.1136/annrheumdis-2021-221996
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#冠状动脉综合征#
80
#长期风险#
84
#综合征#
64
#DMARD#
77