Lancet:EGFR野生型的早期NSCLC患者,免疫治疗获益显著(IMpower010研究)
2021-09-23 网络 网络
在确诊为非小细胞肺癌(NSCLC)的患者中,约50%为局部(I期和II期)或局部晚期(III期)疾病。
在确诊为非小细胞肺癌(NSCLC)的患者中,约50%为局部(I期和II期)或局部晚期(III期)疾病。根治性手术是I-II期和部分IIIA期NSCLC的首选治疗方法。然而,这些早期NSCLC患者的5年生存率有明显差异,IA期患者为92%,IIIA期患者则只有36%。这提示患者体内仍有微转移需要治疗。对于早期NSCLC(IB期[肿瘤≥4 cm]至IIIA期)患者,含铂联合化疗是完全切除术后的辅助治疗标准,但对存活率提升有限(4%-5%)。ADAURA研究表明,奥希替尼(osimertinib)辅助治疗能够为EGFR突变的早期NSCLC患者带来无癌生存获益。而对于大多数EGFR野生型的早期NSCLC患者,仍然迫切需要新的辅助策略。
基于铂类的辅助化疗可使完全肿瘤切除的高危早期NSCLC患者获得5年生存期。近年来,免疫治疗已在晚期NSCLC中取得了显著的成果,并改变了晚期NSCLC的治疗模式。研究者们逐渐将目光转向免疫新辅助/辅助治疗,期待免疫治疗能够为更多早期NSCLC患者带来获益。
免疫疗法已经成为晚期NSCLC一线治疗的基石之一,这类药物是否也能够为早期患者带来获益?
近日,IMpower010研究结果在《柳叶刀》重磅发表。对于手术切除的II-IIIA期NSCLC患者,辅助化疗后继续进行PD-L1抑制剂阿替利珠单抗(atezolizumab)治疗,与最佳支持治疗相比能够显著延长无癌生存期,复发或死亡风险降低21%,PD-L1表达≥1%的患者获益更大,复发或死亡风险降低34%。
论文指出,这是“首批来自IB-IIIA期NSCLC辅助免疫治疗的3期研究数据。”《柳叶刀》同期评论文章指出,“IMpower010代表了胸部肿瘤学的一个重要里程碑。这些发现对可切除的NSCLC患者具有重要意义。”
今年6月,这项研究在美国临床肿瘤学会(ASCO)年会初步发表,当时,ASCO首席医学官Julie R. Gralow博士也表示,“这是我们第一次看到免疫疗法用于治疗早期肺癌是有效的。无论是我们对于免疫疗法的了解,还是对许多肺癌患者来说,这可能都是重要进步。”
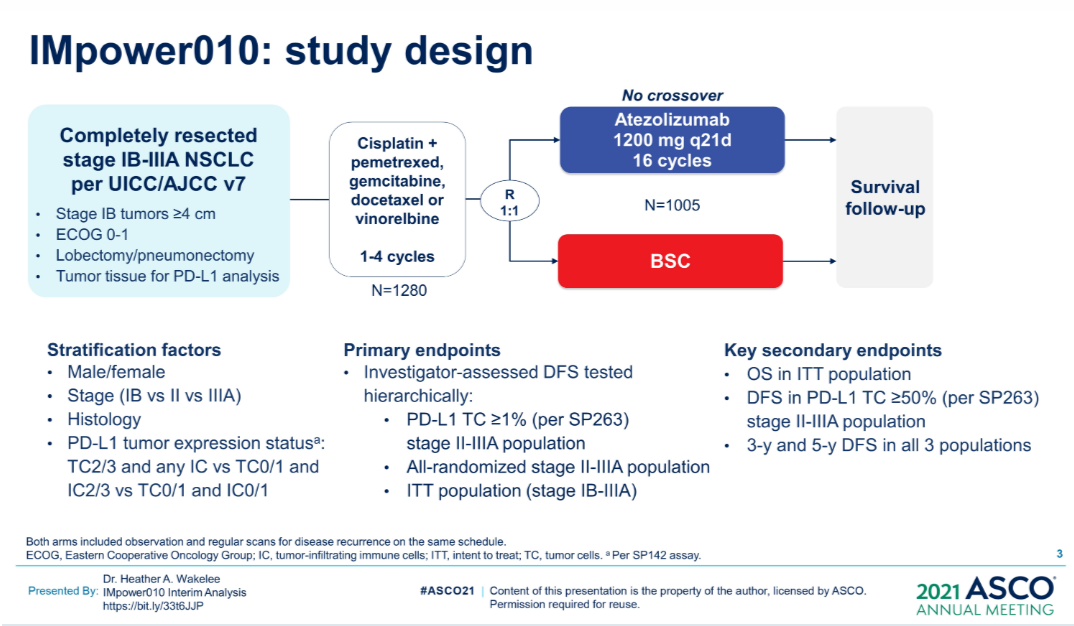
IMpower010是一项随机、多中心、开放标签、3期研究,在全球22个国家和地区的227个临床中心开展。共有1280名IB期(肿瘤≥4 cm)至IIIA期NSCLC患者在完全切除后入组,最终1005名患者在辅助化疗后1:1随机分组接受阿替利珠单抗辅助治疗(n=507)或最佳支持治疗(n=498)。实际每组共495人接受治疗。研究主要终点为无病生存期(DFS)。
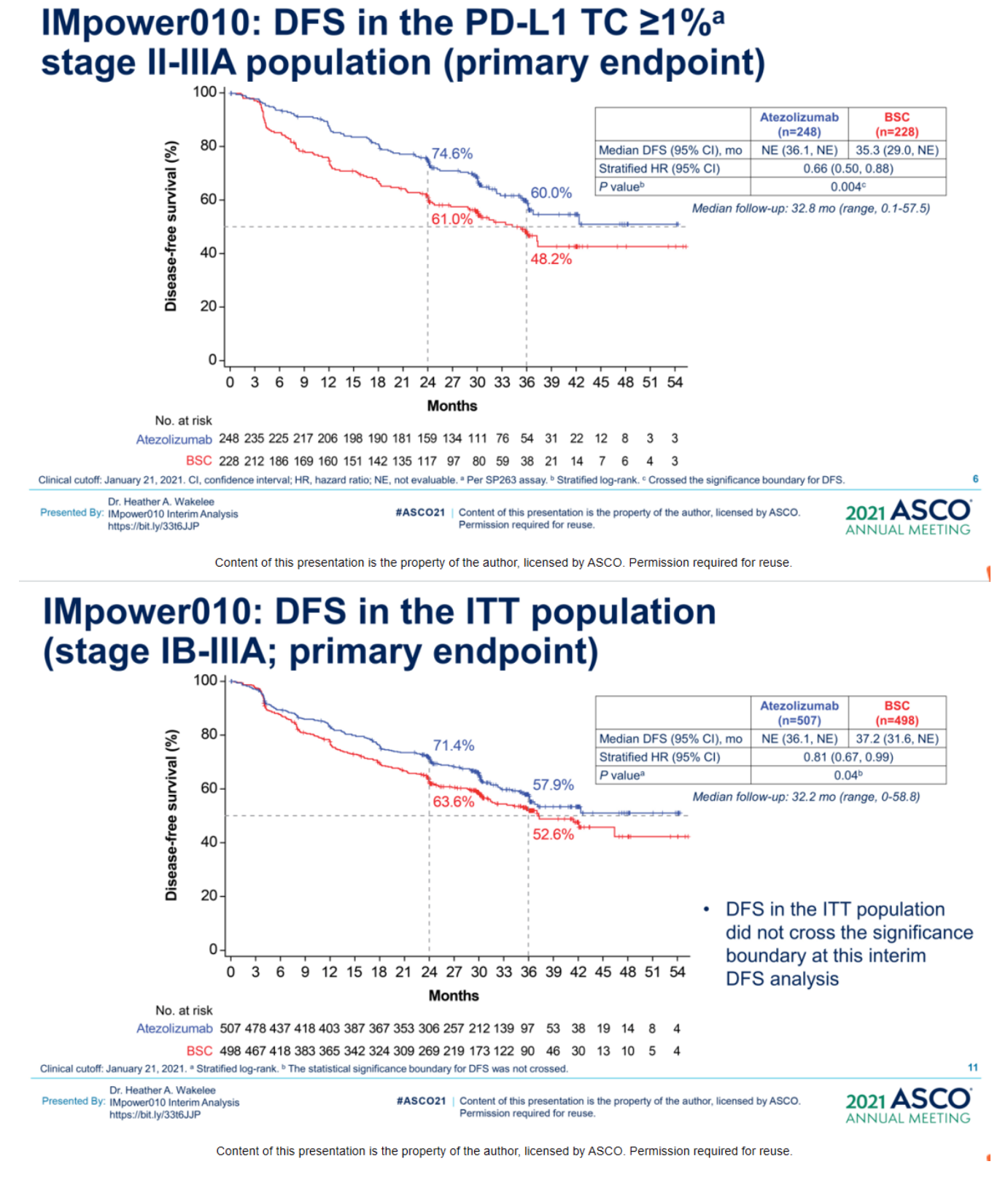
在对II-IIIA期人群中位随访32.2个月后,与最佳支持治疗相比,阿替利珠单抗显著延长了无病生存。
-
PD-L1表达≥1%的II-IIIA期患者:疾病进展或死亡风险降低34%(分层HR 0.66),3年无病生存率更高(60% vs 48%)。
-
所有II-IIIA期患者:疾病进展或死亡风险降低21%(分层HR 0.79),3年无病生存率更高(56% vs 49%)。
-
所有意向治疗人群(IB–IIIA期):疾病进展或死亡风险降低19%(分层HR 0.81),3年无病生存率更高(58% vs 53%)。
-
PD-L1表达≥50%的II-IIIA期患者:初步数据显示死亡风险降低57%(未分层HR 0.43)。
探索性分析中,在II-IIIA期患者中,大多数患者亚组中都能普遍看到阿替利珠单抗的无癌生存优势。
截至分析,5年无病生存率和总体生存的数据都仍在积累中,需要更长时间的随访才能进一步显示阿替利珠单抗辅助治疗的生存获益。
阿替利珠单抗组的中位剂量为16剂(1-16)。阿替利珠单抗组任意级别的AEs发生率为92.7%,而BSC组为70.7%;阿替利珠单抗组3/4级AEs发生率为21.8%,BSC组为11.5%;阿替利珠单抗组5级治疗相关的AEs发生率为0.8%,18.2%的患者因AEs而停用阿替利珠单抗。
不过,鉴于主要结局的积极数据,以及研究没有观察到新的安全信号,论文指出,这表明,对于已切除的II-IIIA期NSCLC患者,辅助化疗后的阿替利珠单抗治疗可能是一种有潜力的治疗选择,可延长患者的无癌生存期,特别是在肿瘤细胞PD-L1表达≥1%、尤其是PD-L1表达≥50%的患者中。
在《柳叶刀》评论文章中,麻省总医院(MGH)Justin F Gainor博士也指出,来自局部晚期、不可切除NSCLC的研究数据提示,疾病控制的延长可能是具有临床意义的总生存期替代指标。接下来紧迫需要更明确识别出最有可能从中获益的患者。IMpower010数据显示,尽管PD-L1表达≥1%的患者获益,但无病生存期的改善似乎主要是由PD-L1≥50%的患者驱动的,尽管这一探索性分析结果需要谨慎解释,但这与晚期疾病中的研究发现一致。
评论文章进一步展望表示,“IMpower010研究代表了向前迈出的重要一步。在不久的将来,随着其他免疫疗法在辅助治疗和新辅助治疗中其他研究结果出炉,可切除NSCLC的治疗前景可能会更复杂。PD-L1抑制剂辅助治疗NSCLC患者的成功,为接下来十年中,免疫检查点抑制剂继续扩展应用于不同疾病辅助治疗打下了基础。”
有关IMpower010研究的讨论
徐嵩教授:IMpower010中,入组了EGFR/ALK阳性的患者,这样设计的原因是什么?
Heather A. Wakelee教授:IMpower010研究设计时,没有任何理由要排除这部分患者,该试验设计时,新药还未出现,因此当时对于这部分患者,并没有其他的标准治疗方案。
EGFR突变NSCLC的情况很复杂,IMpower010所有入组人群中,EGFR突变患者约占11%,亚组分析结果显示,43例PD-L1 TC≥1%的Ⅱ~ⅢA期EGFR突变患者,有DFS的获益趋势,HR为0.57,但95%CI边界值超过1,差异不明显。目前针对EGFR突变患者的辅助靶向治疗Ⅲ期研究均未得出OS阳性结果,只有DFS获益。ADAURA研究可能有所不同,因为其DFS获益非常大。也许EGFR突变伴PD-L1高表达的亚组人群能够从辅助免疫治疗中有生存获益,但结果是否如此目前还不清楚。
周彩存教授:EGFR突变NSCLC的确非常复杂,或许长期吸烟的患者能够从辅助免疫治疗中获益。因此,我们需要分辨哪些患者的PD-L1表达是因为EGFR通路,抗癌管家-康爱管家,我们一起抗癌,治愈癌症不是梦。哪些不是因为EGFR通路,这是转化研究的重点。而且有些EGFR突变为单一突变,有些则存在共突变的情况,共突变患者或许能够从免疫治疗中获益。
徐嵩教授:如何看待免疫治疗对长期生存的影响?IMpower010研究是否有望提升一部分患者的长期生存?
Heather A. Wakelee教授:我们都很看好IMpower010研究能够带来OS获益。根据层级统计学检验,对于PD-L1 TC≥1%的Ⅱ~ⅢA期患者,DFS显著获益且HR为0.66;所有Ⅱ~ⅢA期患者,DFS的HR为0.79,仍然具有显著的统计学意义;接下来我们需要分析所有入组的ⅠB~ⅢA期,目前有DFS的获益趋势,但仍然需要随访,只有当所有人群取得DFS阳性结果后,才能开始分析OS,如何检验这一结果还需讨论。
在PD-L1 TC≥1%的Ⅱ~ⅢA期患者中,两条DFS曲线始终是分开的,治疗持续约12个月,随访时间达到32.2个月,在这中间的20个月随访时间中,两条曲线依然没有重合。我个人很看好阿替利珠单抗辅助治疗能够带来OS的改善,而不仅仅是延长复发时间,DFS对患者很重要,但和治愈是两回事。
周彩存教授:我对IMpower010研究最终会显示OS获益很有信心,纵观所有试验,通过免疫治疗获得DFS并非易事,但我们最终肯定能有OS获益,即使是在小细胞肺癌中,例如CASPIAN研究未显示PFS获益,但OS获益明显,延长有2个月。IMpower010研究的DFS获益非常明显,所以我有信心在1至2年后看到OS获益。阿替利珠单抗辅助治疗组的5年生存率应该会很不错,特别是与辅助化疗相比,因为化疗对5年生存率的改善只有5%。我坚信IMpower010研究未来能够获得OS获益,而且效果要优于化疗。
徐嵩教授:IMpower010研究亚组分析显示ⅢA期患者DFS获益更好,长期的生存结果也会是这样吗?也就是说辅助免疫治疗对ⅢA期患者的疗效优于ⅠB期患者?
Heather A. Wakelee教授:我认为应该注意不要过分解读,但如果真能如此,那肯定很好,我也很希望是这样。ⅢA期患者即使手术和化疗都是最完美的情况下,5年生存率仍不超过50%。而对于ⅠB期患者,是否需要辅助治疗还有争议,当考虑辅助治疗时,理论上而言,手术应该是最有效的手段,但部分患者手术后仍有疾病残留,并且可能复发,分期的意义也在于此。ⅠB期患者基本上通过手术都已经治愈,既然如此,再给他们额外的治疗并不会有什么帮助,我们需要知道哪些患者手术后还需要治疗,哪一种治疗最适合他们。
IMpower010研究中ⅢA期患者获益更多的原因可能在于,这些患者本身复发的风险比ⅠB期患者更高。我们要选择最能够获益的患者,而不是那些已经治愈,获益不大的患者,因为药物都有毒性的风险。能从阿替利珠单抗辅助治疗中获益的患者是符合一定标准的,作为医生,我们要做的就是继续研究新的MRD检测手段,判断哪些患者已经治愈,哪些还需要治疗。
周彩存教授:我也不支持Ⅰ期患者接受辅助治疗,我们只给ⅠB期术后ctDNA阳性的患者进行辅助治疗,ctDNA阳性患者存在复发风险,可以考虑进行辅助免疫治疗。除了疗效,还应当考虑毒性,尤其是经济毒性。因此,我并不建议对ⅠB期术后达到CR的患者使用辅助免疫治疗,应该只用于ctDNA阳性患者。
徐嵩教授:针对早期NSCLC患者,我们是在新辅助治疗阶段,还是在辅助治疗阶段进行免疫治疗?或者术前已经使用免疫治疗,术后是否还要继续?到底哪一种模式最好呢?
Heather A. Wakelee教授:CheckMate-816是一项很重要的研究,因为只有该试验只用了新辅助治疗,其他Ⅲ试验都是新辅助免疫治疗联合化疗+手术+辅助免疫治疗,因此CheckMate-816研究无法直接回答这一问题。在我看来,我们需要考虑如何减少患者不必要的毒性暴露,同时保证最好的疗效。假设医生判断患者的肿瘤便于手术,那就应该进行手术,然后通过MRD检测判断是否需要继续治疗。而对于肿瘤较大或者已经转移的患者,或许新辅助免疫联合化疗是个不错的选择。我觉得等我们拿到现在正在进行的这些临床试验的结果后,我们会有很多数据需要整理。我个人认为,大部分患者可能会先进行手术,术后判断谁需要额外的治疗,然后给予他们远比过去辅助化疗更好的治疗方案。
周彩存教授:我们在跟患者商量可行方案时,患者最开始通常会想尽快手术,手术是首选。CheckMate-816研究取得pCR阳性结果,但我认为pCR率还不够好,需要实现无事件生存的改善,但现在还没有相关数据。因此,我更倾向于使用辅助免疫治疗,在临床实践中可及性更好。如果我们想了解新辅助免疫治疗的效果,可以参考CheckMate-816研究,如果试验结果显示有巨大的获益,比如无事件生存期或长期生存的改善,那我也会做出改变。抗癌管家-康爱管家,我们一起抗癌,治愈癌症不是梦。但现在我更倾向于辅助免疫治疗。现在还有很多试验正在进行之中,我们需要等这些试验出结果,然后再判断哪种模式最好,现在还难以给出答案。目前,IMpower010是首个显示了明显DFS获益的Ⅲ期随机对照试验,DFS获益巨大,而且很有可能实现OS获益,我认为阿替利珠单抗辅助治疗在不远的未来很可能成为标准治疗,我们只要等官方批准即可。
徐嵩教授:未来辅助免疫治疗能够彻底替代辅助化疗的地位吗?
周彩存教授:我认为现阶段无疑还是需要辅助化疗,免疫治疗只对PD-L1高表达的患者有效。免疫治疗和化疗有明显的协同作用,化疗后,免疫治疗的疗效可能进一步提升。也许未来我们会发现更好的免疫疗法,比如新的免疫检查点抑制剂、新的联合方案,其疗效要优于免疫联合化疗,那时便可进入无化疗时代,而现阶段无疑还是需要化疗。
Heather A. Wakelee教授:现阶段我们还是需要辅助化疗,其仍然是标准治疗,也确实能够提高治愈率。我相信未来我们能够知道,哪些患者不需要冒额外化疗的风险,就能保证充分的获益,这需要在毒性风险和潜在获益之间权衡。如果未来研究发现只使用辅助免疫治疗就能获得足够的改善,那我认为这是合理的。而当前即便IMpower010中阿替利珠单抗取得很好的DFS获益,我们也不能下不需要化疗这样的判断,因为试验中每一名患者都接受过辅助化疗。
原始出处:
1.Heather A. Wakelee, et al.IMpower010: Primary results of a phase III global study of atezolizumab versus best supportive care after adjuvant chemotherapy in resected stage IB-IIIA non-small cell lung cancer (NSCLC). 2021 ASCO, abs 8500.
2.Enriqueta Felip,Nasser Altorki, Caicun Zhou, Tibor Csőszi, Ihor Vynnychenko, Oleksandr Goloborodko, et al. Adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB–IIIA non-small-cell lung cancer (IMpower010): a randomised, multicentre, open-label, phase 3 trial. The Lancet, September 20, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#野生型#
86
#Lancet#
59
#SCLC患者#
53
#power#
67
#NSCLC患者#
58
#GFR#
59
#MPO#
73
学习了,谢谢分享
92
旅游的人呢!
101