近年来,肿瘤免疫治疗(Immunology Oncology Therapy, I-O)已成为恶性肿瘤治疗的重要手段之一。肿瘤免疫治疗并不直接攻击癌细胞,而是通过激活人体自身免疫系统来抗击肿瘤,具有良好的安全性及耐受性。PD-1/L1 抗体药物作为肿瘤免疫治疗的代表药物,在恶性肿瘤治疗中取得了巨大的成功。虽然患者用药后初始应答相对较慢,但是一旦从 PD-1/L1 抗体的治疗中产生应答,可以明显提升一部分患者的长期生存率。
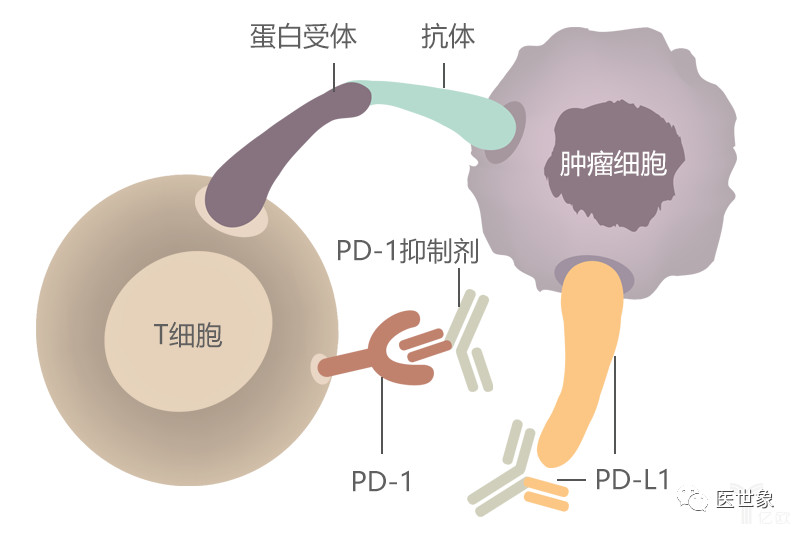
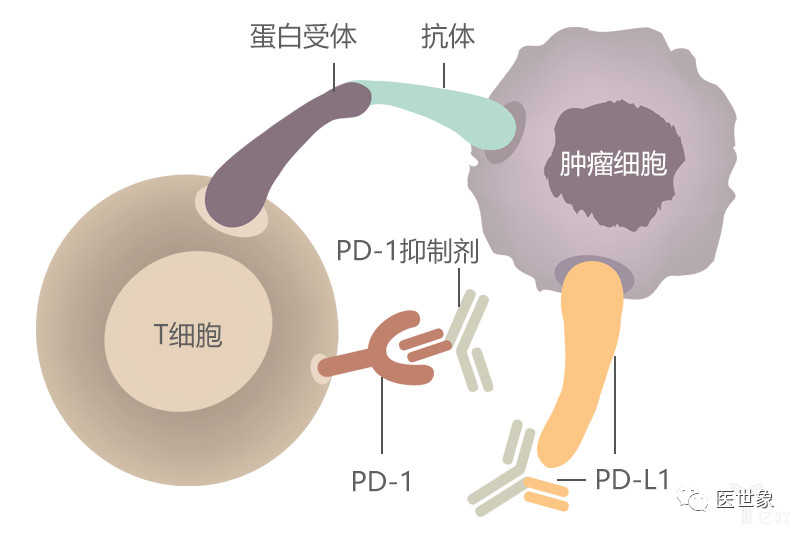
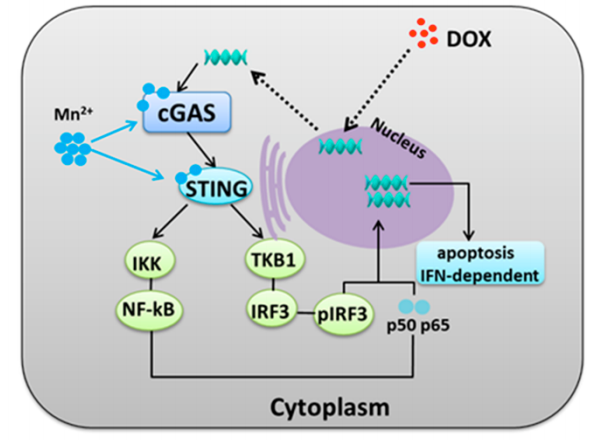
正常情况下,人体内的T细胞可以监测并清除肿瘤细胞。然而,肿瘤细胞非常狡猾,其表面的PD-L1/PD-L2可以与T细胞表面的PD-1结合,影响T细胞功能,使癌细胞躲避免疫系统的攻击。PD-L1配体除了与PD-1结合外,还能以受体形式与CD80配体结合,抑制T细胞活性。
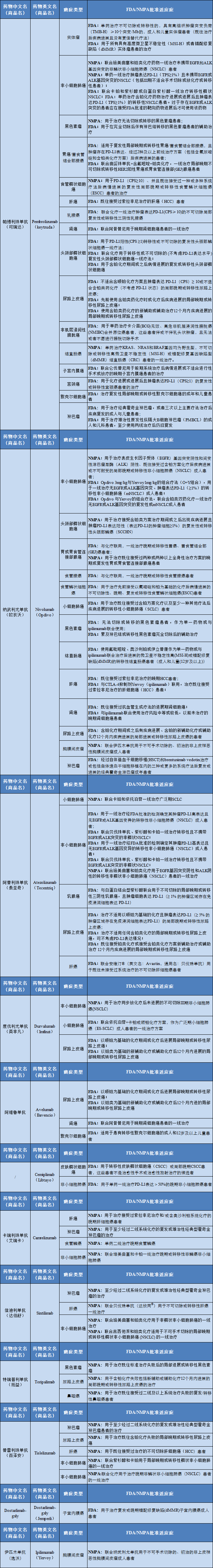
从2014年,全球首款PD-1抑制剂Opdivo问世开始,到目前,已经有多款PD-1/PD-L1药物获批上市,小编根据允英整理的一篇(NMPA/FDA)获批适应症,列举一下哪些恶性肿瘤可以使用PD-1/PD-L1药物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










谢谢分享
78
感谢分享
87
#PD-L1#
73
#适应症#
81
免疫治疗目前在实体瘤的治疗中,愈发重要,安全性的关注同等重要
101
学习了,谢谢
83