JAMA:英夫利昔单抗主动治疗性药物监测方案对免疫介导炎症性疾病患者临床缓解率的影响
2021-05-07 MedSci原创 MedSci原创
对于接受英夫利昔单抗治疗的免疫介导炎症性疾病患者,与标准治疗相比,主动治疗性药物监测方案在30周内没有显著提高患者的临床缓解率

以英夫利昔单抗为代表的肿瘤坏死因子(TNF)抑制剂可治疗许多慢性免疫介导炎症性疾病,如类风湿性关节炎、脊椎关节炎、银屑病关节炎、溃疡性结肠炎、克罗恩病和银屑病,但约有20-55%的患者对生物单抗治疗无应答。主动治疗性药物监测(TDM)是一种基于定期监测血清药物水平的个体化给药方法,可最大限度地提高英夫利昔单抗和其他生物药物的疗效和安全性。近日研究人员考察了基于TDM的英夫利昔单抗治疗方案对临床疗效的影响。

研究在挪威21医院开展,411名类风湿性关节炎、脊椎关节炎、银屑病性关节炎、溃疡性结肠炎、克罗恩病或银屑病患者参与,随机接受基于定期监测血清药物水平,调整药物剂量和治疗间隔的英夫利昔单抗治疗(TDM组;n=207)或标准英夫利昔单抗治疗(标准治疗组;n=204)。研究的主要终点是第30周的临床缓解。
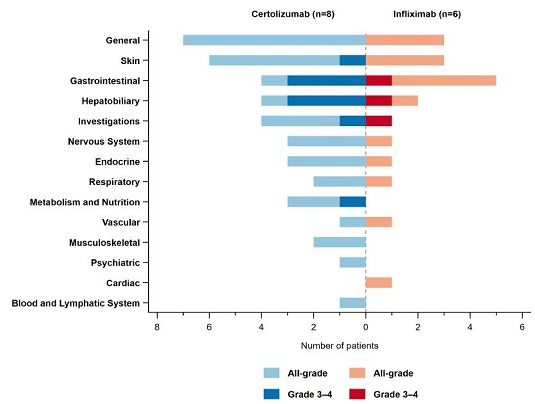
患者平均年龄44.7岁,209名女性(51%),398名(TDM组198名,标准治疗组200名)患者完成随访。TDM组的198名患者中有100名(50.5%)在第30周获得临床缓解,标准治疗组200名患者中有106名(53.0%)在第30周获得临床缓解(调整后的差异为-1.5%)。TDM组和标准治疗组分别有135例(68%)和139例(70%)患者出现不良事件。

对于接受英夫利昔单抗治疗的免疫介导炎症性疾病患者,与标准治疗相比,主动治疗性药物监测方案在30周内没有显著提高患者的临床缓解率。
原始出处
Silje Watterdal Syversen et al. Effect of Therapeutic Drug Monitoring vs Standard Therapy During Infliximab Induction on Disease Remission in Patients With Chronic Immune-Mediated Inflammatory Diseases A Randomized Clinical Trial.JAMA. May 4, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疾病患者#
68
#炎症性疾病#
89
#临床缓解#
99
学习学习。
102
#炎症性#
62
学习了
87
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
84
了解
88