Cancers:家族史和胃癌风险的关系:STOP研究的合并分析
2021-07-31 yd2015 MedSci原创
研究表明,有一代胃癌家族史可增加近2倍的发生胃癌风险,并且表明不同病理类型以及部位的风险不同,为以后的预防提供帮助。
虽然胃癌家族史(FH)与发生胃癌的风险有比较明确的相关性。但是对于病理类型,部位以及相关变量等仍需要进一步的明确。因此,国外研究团队开展了相关的研究,评估家族史(FH)与发生胃癌风险的关系。相关结果发表在Cancers杂志上。

该研究纳入STOP研究中的17项研究,共5946例胃癌患者以及12776例对照组。其中15.8%胃癌患者(n = 942) 以及7.7%对照组(n = 979)有一代亲属胃癌家族史。相对于对照组,胃癌患者中男性比例更高 (63.7% vs. 58.3%), ≥65岁患者更多(50.5% vs. 43.0%)以及更多的较低经济地位患者 (63.9% vs. 52.1%);同时,吸烟患者更多(28.9% vs. 25.8%),喝酒的患者更多(14.5% vs. 10.6%)。
与没有一代胃癌家族史相比,有一代胃癌家族史的胃癌发生风险增加,OR为1.84 (95% CI: 1.64–2.04; I2 = 6.1%, P heterogeneity = 0.383)。
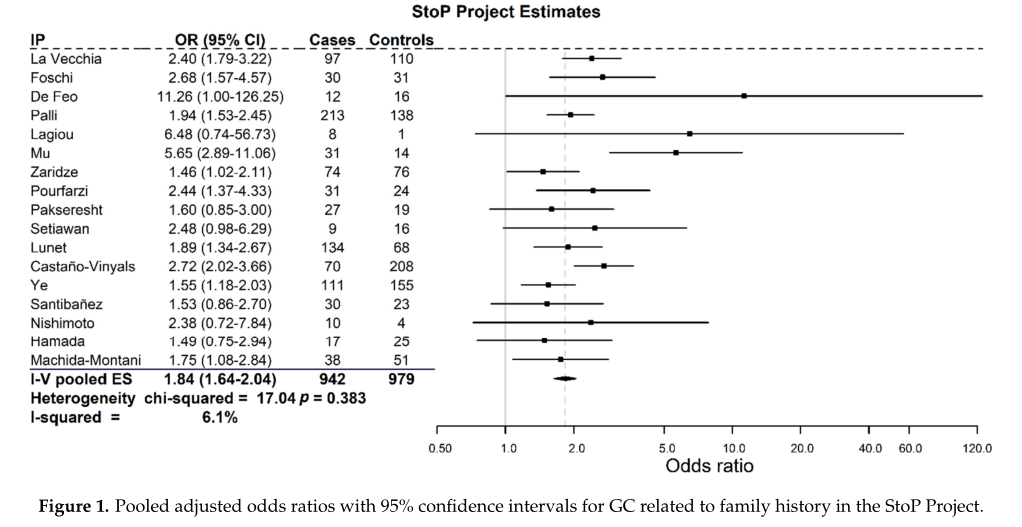
有或无家族史GC风险比
而分析不同家庭成员对发生胃癌风险影响时,有兄弟姐妹胃癌家族史的OR较父母胃癌家族史的高,分别为1.62 (95% CI = 1.20–2.05) 和1.54 (95% CI = 1.28–1.80)。没有观察到显著的异质性差异。
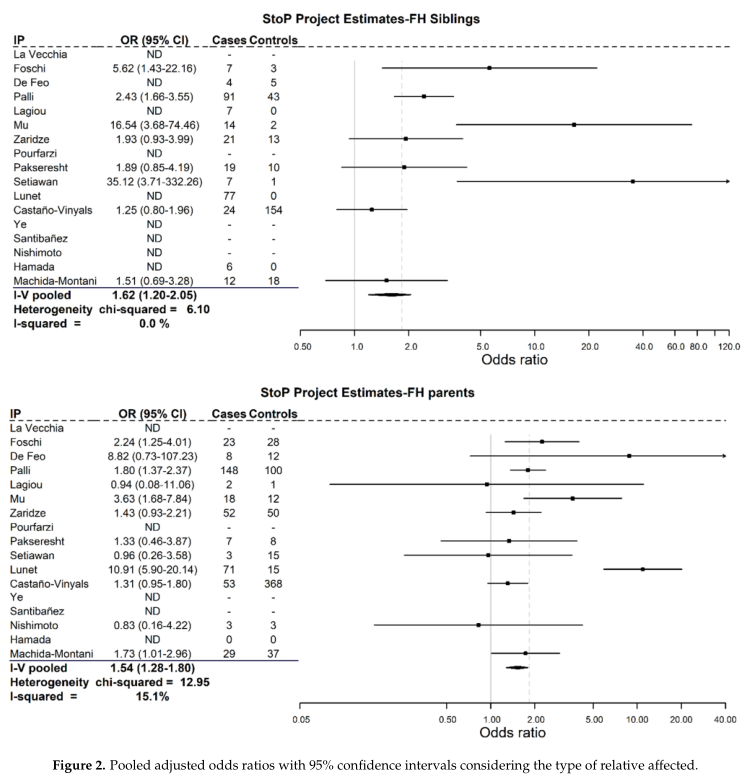
兄弟姐妹或父母GC史的风险比
695例胃贲门GC患者中,92 (13.2%) 患者有一代GC家族史, 而3676例非胃贲门患者有648 (17.6%)例患者有一代GC家族史,合并ORs分别 为1.38 (95% CI = 0.98–1.77) 和1.82 (95% CI = 1.59–2.05)。
同样,2030 例肠型GC患者中, 365 (18.0%)例患者有一代GC家族史,OR 为1.92 (95% CI = 1.62–2.23);1170例弥漫型GC患者中,169 (14.4%)例患者有一代GC家族史,OR为1.62 (95% CI = 1.28–1.96)。
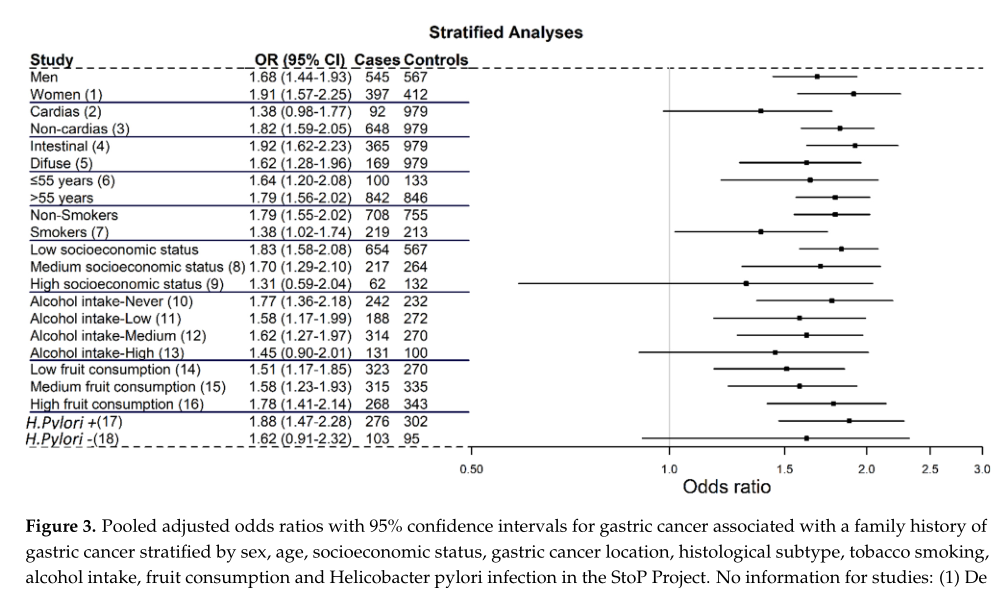
亚组分析GC风险比
而对于年龄、吸烟史、经济地位、饮酒史、水果摄入、幽门螺杆菌感染等亚组分析没有统计学差异。
综上,研究表明,有一代胃癌家族史可增加近2倍的发生胃癌风险,并且表明不同病理类型以及部位的风险不同,为以后的预防提供帮助。
原始出处:
Vitelli-Storelli, F.; Rubín-García, M.; Pelucchi, C.;et al. Family History and Gastric Cancer Risk: A Pooled Investigation in the Stomach Cancer Pooling (STOP) Project Consortium. Cancers 2021, 13, 3844. https:// doi.org/10.3390/cancers13153844.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#风险的关系#
122
#ERS#
77
#癌风险#
75
#家族史#
83
家族史影响好大
83