TGF-β 超家族失调是肺动脉高压的关键
2022-02-14 刘少飞 MedSci原创
转化生长因子-β (TGF-β) 超家族的不平衡信号传导广泛导致 PAH 中血管细胞增殖失调,过度活跃的促增殖 SMAD2/3 信号传导与缺乏的抗增殖 SMAD1/5/8 信号传导一起发生。
TGF-β 超家族具有 30 多种配体,它们共同调节包括脉管系统在内的所有主要器官中的多种发育和稳态过程 。事实上,TGF-β 超家族信号的失调与许多心肌病和血管病有关,包括动脉粥样硬化、血管钙化、马凡综合征、Loeys-Dietz 综合征和遗传性出血性毛细血管扩张症,除了PAH。通常,二聚 TGF-β 超家族配体的结合促进包含两种 I 型和两种 II 型受体丝氨酸/苏氨酸激酶的异四聚体信号复合物的组装。在配体结合后,组成型活性 II 型受体磷酸化 I 型受体,激活 I 型受体胞内激酶结构域。然后信号通过各种规范(涉及 SMAD 转录因子)和非规范(或 SMAD 独立)途径传播。在 PAH 中,最近的证据表明两种主要典型途径之间的信号不平衡,在肺动脉 EC 和 SMC 中,SMAD1/5/8 信号不活跃与 SMAD2/3 信号过度活跃。在其余部分中,我们描述了这种 SMAD 信号失衡如何影响血管重塑的旺盛细胞增殖,并描述了减弱过度 SMAD2/3 信号或恢复患病肺血管系统中缺乏的 SMAD1/5/8 信号的治疗方法。非经典 TGF-β 超家族通路在 PAH 发病机制中的潜在参与知之甚少,但这些信号传导机制与相关的病理状况(如纤维化)有关,值得进一步研究。
TGF-β 超家族失调是 PAH 的关键组成部分
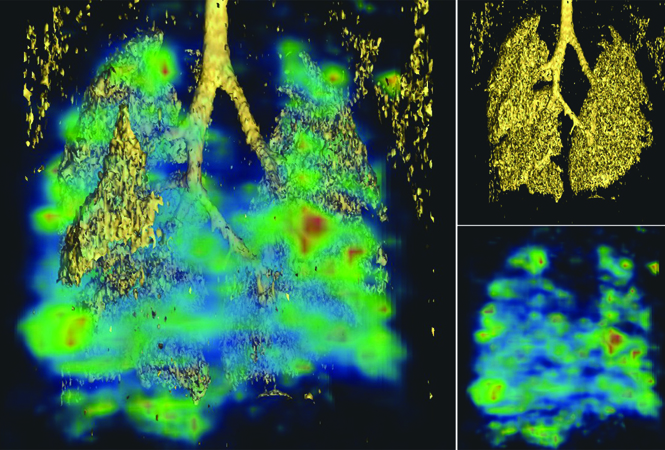
在肺动脉高压 (PAH) 中,病理性血管重塑扭曲了肺动脉脉管系统的大体和微观结构,严重破坏了整个心肺循环的血流模式。原发性病变被认为起源于远端小动脉,其中血管细胞不受控制的增殖导致血管腔变窄和闭塞。管腔空间的损失反过来会增加肺血管阻力和肺动脉压,导致右心室劳损并最终导致心力衰竭。
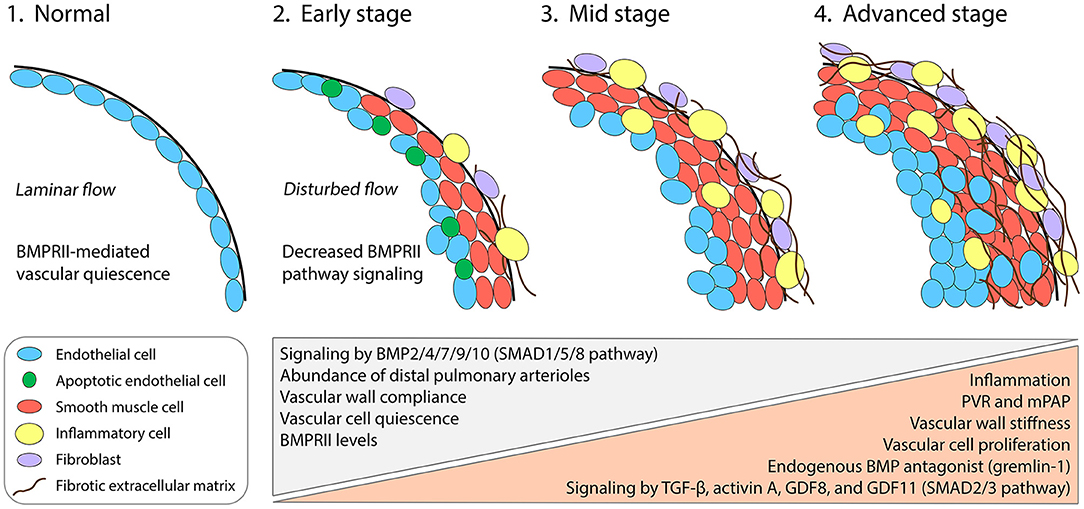
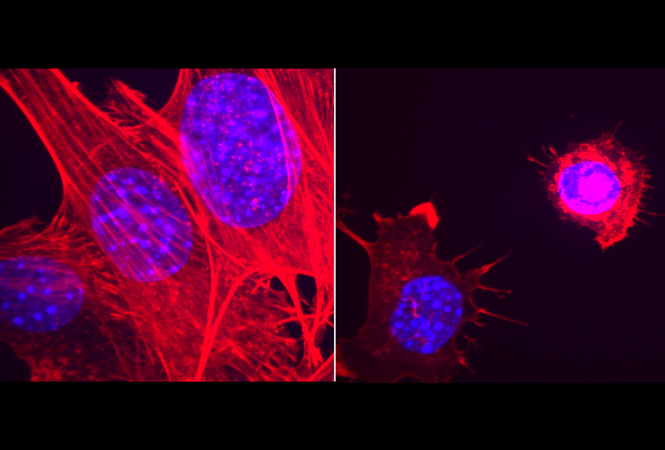
肺动脉壁的多种细胞类型有助于 PAH 中的血管重塑(上图)。平滑肌细胞 (SMC) 过度增殖,从而使血管壁增厚并导致血管肌肉化,包括通常不存在 SMC 的远端小动脉周围。内皮细胞 (EC) 也会过度增殖,并且在疾病的后期会形成阻塞远端小动脉的新内膜病变。因此,针对 SMC 和 EC 的增殖来治疗 PAH 一直是过去二十年来广泛努力的主题。血小板衍生生长因子受体通路的研究,该通路在 PAH 患者的远端肺动脉中强烈上调并导致过度增殖。表明病理学的逆转在临床上是可以实现的—尽管更安全的替代策略是可取的。对 PAH 疾病机制的研究也强调了其他信号转导途径的关键作用,尤其是转化生长因子-β (TGF-β) 超家族的那些,它们与炎症过程和生物力学力相互作用以调节 EC 和 SMC 增殖。
参考文献:
Andre P. Therapeutic Approaches for Treating Pulmonary Arterial Hypertension by Correcting Imbalanced TGF-β Superfamily Signaling. Front Med (Lausanne). 2022 Jan 24;8:814222. doi: 10.3389/fmed.2021.814222. PMID: 35141256; PMCID: PMC8818880.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TGF#
67
#动脉高压#
73
#学习#
104
2021年12月患者无明显诱因下出现发热,Tmax
82
#TGF-β#
115