Eur Urol:前列腺特异性膜抗原放射引导进行挽救性淋巴结清扫治疗患者的肿瘤学结果
2022-06-26 AlexYang MedSci原创
评估了PSMA-RGS挽救性手术的肿瘤学结果,并确定了结果改善的术前预测因素。
对于一部分复发寡转移性前列腺癌(PCa)患者,靶向前列腺特异性膜抗原(PSMA)放射引导(PSMA-RGS)的挽救性手术可能存在治疗价值。近期,来自德国的研究人员在《Eur Urol》杂志上发表文章,评估了PSMA-RGS挽救性手术的肿瘤学结果,并确定了结果改善的术前预测因素。
研究包括了两个三级护理中心(2014-2020年)中,前列腺癌根治术后生化复发(BCR)的患者,并且这些患者进行了PSMA正电子发射断层成像(PET),采用了PSMA-RGS治疗。 研究的干预措施为PSMA-RGS。
研究人员采用Kaplan-Meier和多变量Cox回归模型来评估无BCR(BFS)和无治疗(TFS)的生存率。术后并发症根据Clavien-Dindo进行分类。
研究总共评估了364名没有伴随治疗的患者。在PSMA-RGS,343名(94%)患者的转移性软组织PCa病灶被切除。在PSMA-RGS后2-16周中,165名患者的前列腺特异性抗原(PSA)水平达到<0.2 ng/ml。在3个月内,有24名(6.6%)患者患有Clavien-Dindo并发症,等级为III-IV级。治疗2年时,BFS和TFS率分别为32%和58%。在多变量分析中,术前PSA较高(危险比[HR]:1.07,95%置信区间[CI]:1.02-1.12),PSMA-avid病变数量较多(HR:1.23,CI:1.08-1. 40)、多重(盆腔加腹膜后)定位(HR:1.90,CI:1.23-2.95)、术前影像学中病灶的腹膜后定位(HR:2.04,CI:1.31-3.18)是PSMA-RGS后BCR的独立预测因素。研究的主要局限是缺乏对照组。
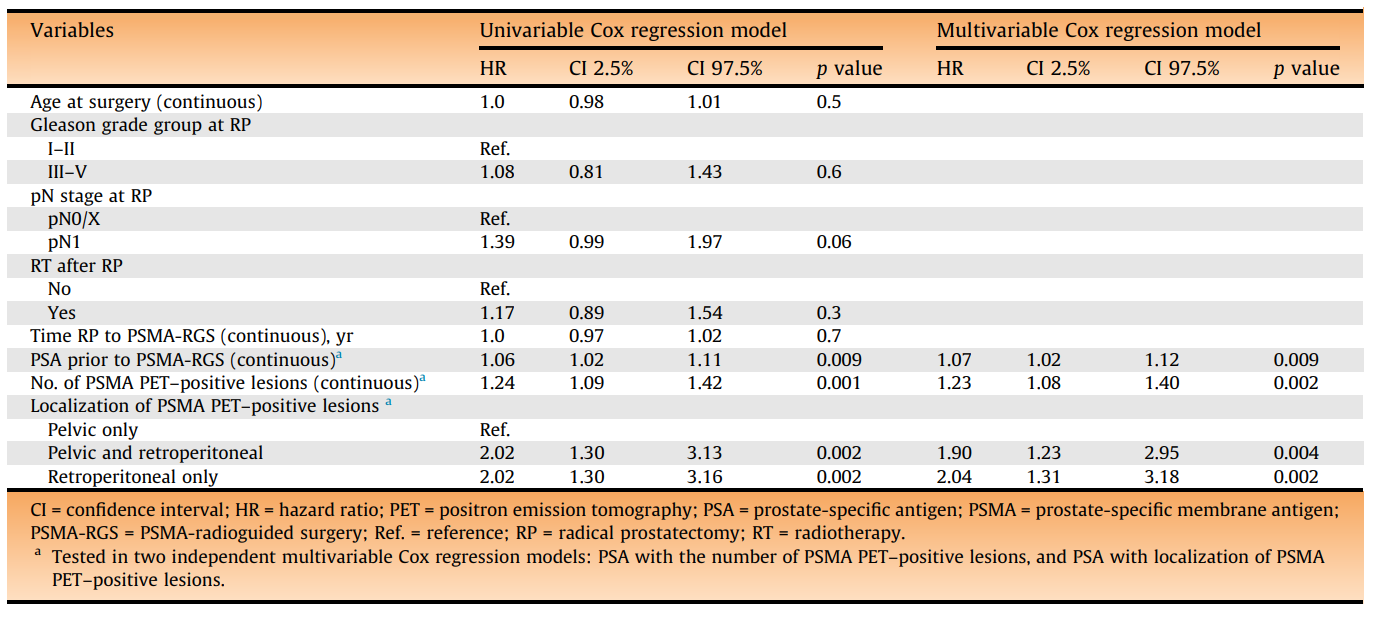
单变量和多变量Cox回归模型预测无生化复发生存
总的来说,在寡复发性PCa中,挽救性手术已成为一种实验性的治疗方法,因此必须根据预期寿命、低PSA值和低数量的位于盆腔的PSMA PET-avid病变来仔细选择要进行挽救性手术的患者。
原始出处:
Sophie Knipper , Mehrdad Mehdi Irai , Ricarda Simon et al. Cohort Study of Oligorecurrent Prostate Cancer Patients: Oncological Outcomes of Patients Treated with Salvage Lymph Node Dissection via Prostate-specific Membrane Antigen-radioguided Surgery. Eur Urol. Jun 2022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#淋巴结清扫#
85
#特异性#
77
#前列腺特异性膜抗原#
93
#淋巴结#
100
#肿瘤学#
88
#抗原#
84