Nature:胰腺癌循环肿瘤细胞转移的Wnt信号
2012-07-10 Beyond 生物谷
循环肿瘤细胞(circulating tumor cell),通常把进入人体外周血的肿瘤细胞称为循环肿瘤细胞。循环肿瘤细胞的检测可有效地应用于体外早期诊断,化疗药物的快速评估,个体化治疗包括临川筛药、耐药性的检测,肿瘤复发的监测以及肿瘤新药物的开发等。 循环肿瘤细胞(CTCs)从原发位肿瘤组织脱落进入血流,启动远端转移过程。尽管循环肿瘤细胞的数量是非常少的,但这些细胞通过特定的细胞信号通路导致肿
循环肿瘤细胞(circulating tumor cell),通常把进入人体外周血的肿瘤细胞称为循环肿瘤细胞。循环肿瘤细胞的检测可有效地应用于体外早期诊断,化疗药物的快速评估,个体化治疗包括临川筛药、耐药性的检测,肿瘤复发的监测以及肿瘤新药物的开发等。
循环肿瘤细胞(CTCs)从原发位肿瘤组织脱落进入血流,启动远端转移过程。尽管循环肿瘤细胞的数量是非常少的,但这些细胞通过特定的细胞信号通路导致肿瘤细胞的血源性传播。
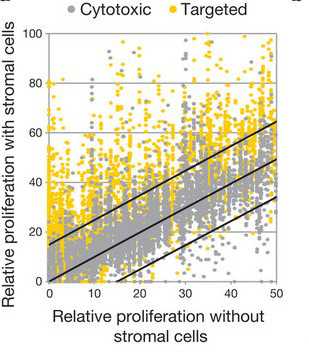
近日发表在Nature杂志上一项研究采用微设备高效捕获老鼠内源性胰腺癌模型中CTCs,并将这些细胞进行单分子RNA测序,发现Wnt2是CTC的候选基因,在循环肿瘤细胞内高度表达。
胰腺癌细胞表达Wnt2后,肿瘤细胞的失巢凋亡现象被抑制,肿瘤细胞体内转移的倾向增加。这种效应与纤维连接蛋白上调以及MAP3K7(也称为TAK1蛋白)激酶受到抑制有关。临床数据也显示511例胰腺癌患者的CTC中发现了Wnt信号高表达。因此,进一步进行分子分析循环肿瘤细胞确定候选的治疗靶标以防止远端癌蔓延是非常有必要的。

doi:10.1038/nature11217
PMC:
PMID:
RNA sequencing of pancreatic circulating tumour cells implicates WNT signalling in metastasis
Min Yu,David T. Ting,Shannon L. Stott,Ben S. Wittner,Fatih Ozsolak,Suchismita Paul,Jordan C. Ciciliano,Malgorzata E. Smas,et al.
Circulating tumour cells (CTCs) shed into blood from primary cancers include putative precursors that initiate distal metastases1. Although these cells are extraordinarily rare, they may identify cellular pathways contributing to the blood-borne dissemination of cancer. Here, we adapted a microfluidic device2 for efficient capture of CTCs from an endogenous mouse…
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Wnt信号#
53
#Nat#
43
#肿瘤细胞#
52
#细胞转移#
62
#循环肿瘤细胞#
61
#WNT#
44