脑实质内炎性假瘤伴高IgG4血症、IgG4阳性浆细胞浸润一例
2020-01-15 张竹青 付伟伟 王明慧 磁共振成像
患者男,29岁,因“双眼颞侧视野缺损1月余”于2016年12月13日就诊,行颅脑MRI检查发现脑内多发异常信号灶,增强扫描示病灶部分强化(图1),临床诊断考虑为脑内炎性病变,给予激素减轻脑水肿等对症治疗后症状明显缓解后出院。4个月后患者诉“记忆力下降1个月,5 d前因酒后头部胀痛,休息不能缓解”于2017年4月12日再次入院就诊。次日行颅脑MR平扫显示原脑内病灶较前范围增大,以左额叶病灶进展尤为显
患者男,29岁,因“双眼颞侧视野缺损1月余”于2016年12月13日就诊,行颅脑MRI检查发现脑内多发异常信号灶,增强扫描示病灶部分强化(图1),临床诊断考虑为脑内炎性病变,给予激素减轻脑水肿等对症治疗后症状明显缓解后出院。4个月后患者诉“记忆力下降1个月,5 d前因酒后头部胀痛,休息不能缓解”于2017年4月12日再次入院就诊。次日行颅脑MR平扫显示原脑内病灶较前范围增大,以左额叶病灶进展尤为显著(图2),MR增强成像示左额叶病灶呈“花环状”强化。影像拟诊为“左额叶病灶考虑胶质母细胞瘤可能”。体检未见明显异常。
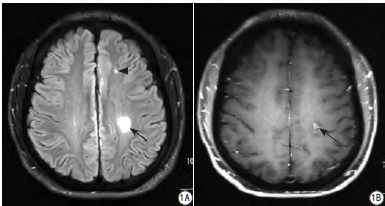
图1 患者颅脑MR平扫和增强扫描。A:FLAIR像显示左侧额叶(黑箭头)、左侧顶叶深部(黑箭)多发高信号影;B:增强扫描左顶叶病灶(黑箭)呈不均匀强化
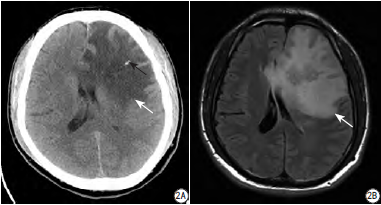
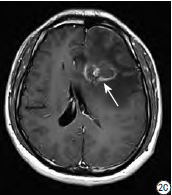
图2 患者颅脑CT和MR。左侧额叶病灶较前范围增大。A:颅脑CT平扫示左侧额顶叶病灶呈低密度(白箭),病灶内见斑点状钙化(黑箭);B:FLAIR显示病灶周围见大片水肿带(白箭);C:MR增强扫描示病灶呈环形强化(白箭)
家族史:父亲体健,母亲38岁时因“走路不稳”检查发现“脑内占位”,病理诊断为“高级别胶质瘤”,放射治疗后占位消失(图3)。

图3 患者母亲颅脑CT及MR。A、B:考虑为“高级别胶质瘤”;C:放疗1年后病灶消失
实验室检查:4月15日肝功示轻度异常:谷草转氨酶AST 90 U/L (正常值范围15~40 U/L),谷丙转氨酶ALT 163.0 U/L(正常值范围9~50 U/L),谷氨酰转肽酶γ-GT 129 U/L(正常值范围10~60 U/L),碱性磷酸酶ALP 192 U/L (正常值范围45~125 U/L),余实验室检查未见特殊。
4月17日行腹部超声检查示肝形态略增大伴肝内回声粗糙,考虑肝炎表现,遂给予脱水及保肝等治疗。4月21日腹部CT平扫示肝左叶形态饱满(图4)。4月22日复查肝功示仍异常,且ALT与γ-GT呈进行性升高,继续行积极保肝治疗。患者入院2周后诉症状未见明显改善,仍有头痛;4月25日复查颅脑MR平扫及增强扫描病灶较前变化不明显,复查肝功示ALP较前明显升高。
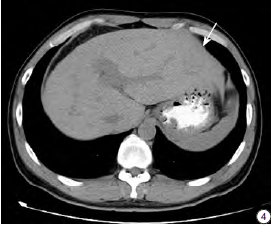
图4 患者腹部CT平扫,示肝左叶形态饱满(白箭)
4月29日患者头痛加剧,查颅脑CT示左额叶病灶呈低密度,伴病灶内见点状钙化(图2A),结合MRI检查,影像考虑非肿瘤性病变,不除外脱髓鞘假瘤可能。为进一步明确病灶性质,于5月5日行开颅脑内病灶切除术,病理提示符合脱髓鞘假瘤表现。术后第3日(5月8日)患者诉无头痛头晕,进食及睡眠改善。5月12日行血清免疫球蛋白测定示IgE 607.30 IU/ml(正常范围0~100 IU/ml),IgG 9.82 g/L(正常值范围7~16 g/L),IgG4 3.04 g/L(正常值范围0.03~2.01 g/L),患者自诉无明显异常症状后出院,嘱继续保肝及抗炎治疗(甲强龙口服)。
5月19日患者于术后半月因头痛4 d第三次入院。查体未见异常。给予甘露醇降颅压及甲强龙抗炎治疗后患者症状缓解。5月22日复查IgG4 2.25 g/L;肝功示ALT 129.0 U/L,AST 73.7 U/L;肝病相关自身抗体测定:抗核抗体ANA弱阳性,抗核颗粒蛋白抗体(印迹法):sp100阳性(++),其余未见异常。5月30日再次复查肝功示ALT进一步升高。结合患者IgG4水平升高、肝功持续异常及肝脏影像学异常,考虑患者存在自身免疫性疾病可能,遂将脑术后病理组织补做IgG4相关免疫组化,结果显示血管周IgG4+浆细胞约10~15/HPF,IgG4+/IgG+约50% (图5)。同时经北京宣武医院病理科病理切片会诊,本例符合脑炎性假瘤的病理表现。
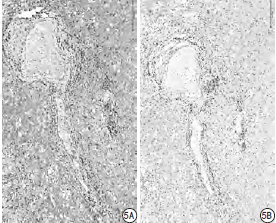
图5 患者脑组织检查免疫组化结果。A为IgG,B为IgG4。IgG4/IgG比值>40%,以及每个高倍视野下IgG4阳性浆细胞数>10个
鉴于目前尚无脑实质内IgG4相关性炎性假瘤的报道,综合以上本例诊断为脑实质内炎性假瘤伴高IgG4血症、IgG4阳性浆细胞浸润。6月2日肝脏穿刺活检病理示肝细胞浊肿、淤胆,少量脂肪变性,汇管区少量炎细胞浸润,呈肝炎表现,免疫组化示IgG与IgG4均为阴性。经积极保肝治疗后转氨酶恢复正常,患者症状好转后出院,激素改为口服继续治疗原发病。患者出院后半年间维持甲强龙抗炎、偶辅以环磷酰胺抗免疫等治疗,于我院门诊多次复查期间无头痛、头晕等症状发作,腹部无不适,2018年1月24日复查颅脑MRI显示颅内病灶较前明显减小(图6)。
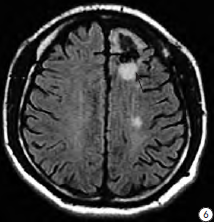
图6 患者甲强龙治疗半年后复查颅脑MR平扫。FLAIR序列示左侧额叶病灶术后示胶质增生(黑箭)
讨论
IgG4相关性疾病(IgG4-RD)是一种少见的自身免疫性疾病,其机制尚不明确,以血清IgG4水平升高、IgG4阳性浆细胞浸润多种组织或器官为特点。该疾病首次于2001年由Hamano等报道,表现为慢性胰腺炎,IgG4相关性疾病几乎可以累及全身各个器官或组织,以胰腺受累最为常见。神经系统亦可受累,但多表现为肥厚性硬膜炎和垂体炎,可同时伴有或不伴有其它器官受累。经检索发生于脑实质内的炎性假瘤伴血清IgG4水平升高的病例截止目前仅发现1例报道。
目前较广为认可的IgG4-RD诊断标准是日本学者提出的,包括3个方面:(1)临床检查显示1个或多个脏器特征性的弥漫性/局限性肿大或肿块形成。(2)血液学检查显示血清IgG4>1.35g/L。(3)组织学检查显示:①大量淋巴细胞和浆细胞浸润,伴纤维化;②组织中浸润的IgG4阳性浆细胞/IgG阳性浆细胞>40%,且每高倍镜视野下IgG4阳性浆细胞>10个。确诊条件:(1)+(2)+(3),可能的诊断诊断:(1)+(3),可疑诊断:(1)+(2)。
本例患者已满足确诊IgG4-RD所需的(1)+(2)及(3)中除伴纤维化以外的所有主要指标;且复习相关文献发现炎性假瘤的诊断主要依靠病理诊断,目前尚无公认的组织学分型,有学者提出根据其纤维化程度的高低将其分为三型:淋巴细胞浸润型、硬化型及混合型;同时,目前国内外报道的少数几例脑实质内炎性假瘤病例中,其病理学上大多亦未提示伴明显纤维化的特点,而非脑实质起源(如硬脑膜)或累及硬脑膜的炎性假瘤病例报道中常伴有纤维化;另外,上文提及的IgG4-RD参考诊断标准的制定依据绝大多数来源于脑实质外的全身各个器官如肝脏、胰腺等,源于脑实质的目前仅有1例报道,其病理学结果亦未发现纤维化的情况与本例类似。故有理由认为,与全身其他系统器官组织相比,鉴于脑实质组织结构的特殊性(脑组织损伤时由星形胶质细胞产生胶质纤维进行修补愈合,而不产生胶原纤维及相应间质蛋白),因此纤维化可能并非脑实质内的炎性假瘤的必需病理诊断依据。
同理,作为IgG4相关的脑实质内炎性假瘤,纤维化可能亦非其必备病理诊断依据。这也是本文中我们通过文献复习拟提出的观点,也希望将来有更多的类似病例来证实。炎性假瘤也称为炎性成肌细胞瘤、浆细胞肉芽肿等,为罕见的软组织炎性病变,病理改变为瘤样病变内淋巴细胞、浆细胞、巨噬细胞及泡沫细胞的浸润。炎性假瘤可以累及全身各个系统,如肺、肝脏、肠系膜等,发生于头颈部时多表现为眶内病变,发生于中枢神经系统的炎性假瘤则极为罕见,目前全球报道仅70余例,一般位于鞍区、鞍旁、脉络丛及脑实质内等,具有一定的侵袭性,常引起颅骨骨质破坏和神经麻痹等症状。
炎性假瘤的发病机制未明,多认为继发于其他疾病,如外伤、细菌或病毒感染、免疫功能障碍等。脑实质内炎性假瘤的影像学表现不典型,主要表现为脑实质的占位性病变,伴或不伴周围脑组织水肿、脑实质侵犯征等表现,与肿瘤性病变难以鉴别,最终确诊仍依赖于病理学诊断。本例患者及其母亲病变均由于其典型的花环状强化而被误诊为高级别胶质瘤,CT平扫对于肿瘤与非肿瘤性病变的鉴别具有较高的诊断价值。一般而言,高级别胶质瘤由于肿瘤细胞排列较为密集,故影像学上CT平扫上多呈等、高密度表现,且罕有伴钙化,而炎性假瘤以炎性细胞浸润为主要病理特征,CT平扫多呈等低密度,且可以出现钙化,由此提示病变可能为非肿瘤性病变而非高级别胶质瘤。
对于非肿瘤病变中,本病还需与瘤样脱髓鞘病变(既往也称瘤样脱髓鞘病或脱髓鞘假瘤)进行鉴别,但在瘤样脱髓鞘病变中罕有伴钙化者的文献报道,由此可以排除脱髓鞘假瘤的诊断。同时复习文献发现有数例脑实质炎性假瘤提到CT图像上显示钙化改变,且炎性假瘤的组织病理学中也可偶见砂粒体样钙化的报道,由此推测钙化在炎性假瘤的影像学诊断具有一定的价值。鉴于其罕见性,本文报道的脑实质内炎性假瘤在病灶密度及钙化等特点尚需更多的病例报道进一步总结证实。对本例患者肿瘤与非肿瘤的鉴别决定不同的治疗方案,对患者的预后及生存质量具有重大意义。
对于IgG4疾病的治疗,其一般对糖皮质醇激素治疗敏感,很多管理指南强调了糖皮质激素作为一线药物的治疗作用,且已有多例经糖皮质激素治疗后症状缓解的报道,本例患者在应用激素治疗后症状缓解无复发,半年后复查MRI显示脑内病灶较前明显好转(图5)。但是有学者回顾分析应用糖皮质激素复发率高达72%,同时有的学者提出糖皮质激素的毒副作用对60岁以上的患者尤为突出,由此呼吁免疫抑制剂与针对性免疫调节剂的应用对于减少或替代老年患者糖皮质激素的使用有着重要意义。
原始出处:
张竹青,付伟伟,王明慧,等.脑实质内炎性假瘤伴高IgG4血症、IgG4阳性浆细胞浸润一例报告并文献复习[J].磁共振成像,2019(01):53-56.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









厉害了
112
#炎性假瘤#
90
#脑实质#
65
#IgG4阳性浆细胞#
73
#浆细胞#
99
#IgG4#
77
#IgG#
0
非常好的病例!
130