Eur Urol:评估两种起始剂量的乐伐替尼加依维莫司对肾细胞癌患者的安全性和有效性:一项随机的2期试验
2022-04-11 AlexYang MedSci原创
评估了较低起始剂量的乐伐替尼是否具有与之相当的疗效,且能同时改善乐伐替尼加依维莫司治疗晚期RCC患者的耐受性。
乐伐替尼(18毫克)加依维莫司(5毫克)被批准用于先前接受过一种或多种抗血管生成疗法的晚期肾细胞癌(RCC)患者。近日,来自美国加州希望之城综合癌症中心等单位的研究人员评估了较低起始剂量的乐伐替尼是否具有与之相当的疗效,且能同时改善乐伐替尼加依维莫司治疗晚期RCC患者的耐受性。相关研究结果发表在EUROPEAN UROLOGY期刊上。

这是一项在晚期透明细胞RCC患者中进行的随机、开放标签的2期全球试验。这些患者在之前的一次血管内皮生长因子靶向治疗(之前所允许的抗程序性死亡-1/程序性死亡配体-1治疗)后出现疾病进展。
患者被以1:1的比例随机分配到14或18毫克的乐伐替尼起始剂量,均与依维莫司 5 mg/d联合使用。14毫克组的患者将在第2周期第1天升至乐伐替尼18毫克,除非有2级不耐受或任何≥3级的需要减少剂量的治疗诱发不良事件(TEAEs)在第一个28 天的周期中出现。
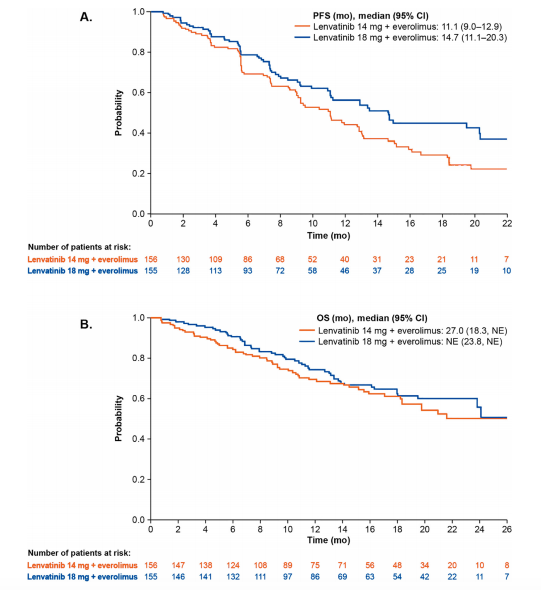
图1 Kaplan-Meier存活曲线
研究的主要疗效终点是研究者评估的截至第24周的客观反应率(ORRwk24);14毫克组与18毫克组的非劣效阈值为P≤0.045。主要安全终点是24周内随机出现不耐受2级或任何≥3级TEAEs的患者比例。
结果表明,14毫克组的ORRwk24(32%[95%置信区间{CI}25-39])并不非劣效于18毫克组的ORRwk24(35%[95%CI 27-42];优势比:0.88;90%CI 0.59-1.32;P = 0.3)。不耐受2级或任何≥3级TEAEs的比例在两组之间相似(14毫克,83% vs 18毫克,80%;p = 0.5)。总ORR、无进展生存期和总生存期等次要终点在数值上18毫克组更有优势。本研究的一个局限性是,研究设计不允许对治疗组之间的无进展生存进行全面比较。
综上所述,该研究结果支持已批准的晚期RCC患者每天服用18毫克乐伐替尼加5毫克依维莫司的剂量方案。
原始出处:
Pal SK, Puente J, Heng DYC, et al. Assessing the Safety and Efficacy of Two Starting Doses of Lenvatinib Plus Everolimus in Patients with Renal Cell Carcinoma: A Randomized Phase 2 Trial. Eur Urol. 2022 Feb 21.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#细胞癌#
85
#安全性和有效性#
92
学习到了
105
学习一下
84
认真学习了
103