Blood:遗传-转录组学分析明确关键转录因子是人红白血病的驱动因素
2020-05-12 QQY MedSci原创
急性红细胞白血病(AML-M6或AEL) 是一种罕见的侵袭性血液恶性肿瘤。既往研究表明,AEL白血病细胞通常携带已知的AML相关癌基因的复杂核型和突变。
为了更好地定义驱动红系表型的潜在分子机制,研究人员对33例AEL样本系列进行研究,这些样本代表了AEL的三个遗传亚组,包括TP53突变、表观遗传调控子突变(如DNMT3A、TET2或IDH2)和未定义的低突变负荷的病例。
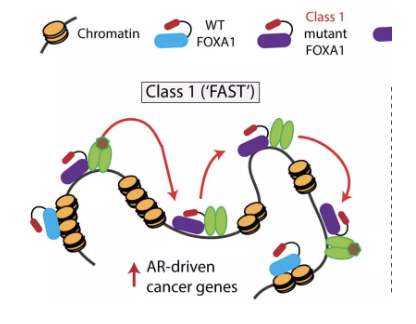
研究人员建立了一个基于红系 vs 髓系的转录组学的“空间”,在该“空间”中,与上述分子亚组无关,大多数AEL样品表现出与非M6 AML和骨髓增生异常综合征样品不同的独特定位。值得注意的是,超过25%的AEL患者(包括在基因上不确定的亚组中)显示出关键转录调节因子的异常表达,包括SKI、ERG和ETO2。这些因子在小鼠红系前体细胞中的异位表达阻碍了红系体外分化,导致永生化,与GATA1结合位点的染色质可及性降低以及对GATA1活性的功能干扰有关。
体内模型显示,致命的红系、红系/髓样混合或其他恶性肿瘤的发生,取决于表达AEL相关变异的细胞群。
总而言之,本研究提示,AEL是一种具有红系同一性的分子异质性疾病,部分原因是造血干细胞或祖细胞中关键的红系转录因子的异常活性。
原始出处:
Alexandre Fagnan,et al. Human erythroleukemia genetics and transcriptomes identify master transcription factors as functional disease drivers. Blood. April 29, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#转录#
60
#驱动因素#
0
#转录组#
0
#转录因子#
132