刘育:左心耳封堵预防心房颤动患者卒中的研究进展
2017-01-10 刘育 365医学网
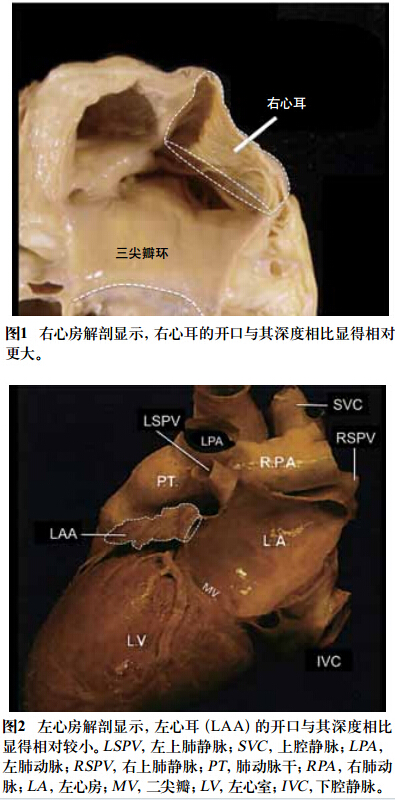
心房颤动(房颤)是临床上常见的心律失常。卒中是房颤患者危害最大的并发症,显著增加致残率和致死率。研究表明,左心耳是房颤患者血栓形成的重要部位,瓣膜性房颤患者约60%的血栓起源于左心耳,非瓣膜性房颤患者90%的血栓来自左心耳。经过十余年的快速发展,左心耳封堵术已成为房颤患者预防卒中的重要方法。一、左心耳与房颤卒中 左心耳是胚胎时期原始左心房的残余,呈狭长、弯曲的管状结构。窦性心律患者左心耳大多
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习了。。
83
#研究进展#
55
#左心耳#
59
#心房#
57
学习了,很好
90
左心耳封堵术已成为房颤患者预防卒中的重要方法。
82