Lancet:牛津大学研究发现“非典型小卒中”的危害大到你想不到
2021-03-06 MedSci原创 MedSci原创
与典型TIA发作相比,非典型TIA发作患者具有较高的早期和长期中风风险。将症状不典型的患者考虑入内后,TIA诊断将增加约50%。
短暂性脑缺血发作(TIA),又称为“小卒中”,约有高达25%的卒中是由TIA引起的。TIA发作后卒中的早期风险很高,因此往往需要细致的检查和强化治疗。为了降低早期复发性卒中的风险,TIA常需要同时使用阿司匹林和氯吡格雷两种抗血小板药物治疗,简称双抗。
TIA发病一般无先兆,有一过性的神经系统定位体征,但无责任病灶的证据。由于患者往往在24小时内完全恢复,无后遗症,因此TIA被俗称为“小中风”。然而,既往的研究认为,TIA患者早期发生卒中的风险很高, TIA发病90天内不仅脑梗死发生率升高(10%-20%),同时心肌梗死和猝死的风险也提升,因此目前一致将90天视为脑梗风险“高危期”。
前期,发表在JAMA上的研究则认为,TIA后发生卒中的风险显著增加,30.8%、39%、48.5%的卒中分别发生在TIA后30天、90天与1年以上。其中,卒中发生的中位时间为1.6年。因此,对此类患者的卒中监测时间应延长至90天后。
此外,由于不少TIA患者在影像学检查中未必能观察到急性缺血的表现,基于症状的诊断在临床实践中仍然很普遍。然而,对于“非典型”症状仍然缺乏共识,相关诊断存在挑战,更有大量患者可能没有得到规范治疗。
为此,来自牛津大学血管研究团队的专家对症状不典型的TIA患者和症状典型的TIA患者是否具有相似的后续中风风险和长期风险进行了评估,发现一些不典型、尚未达成诊断共识的症状同样值得关注,以免错过后续治疗和预防。结果发表在最新的Lancet杂志上。
研究人员前瞻性地调查了来自英国牛津郡的92728人的所有中风和突发短暂性神经症状。根据二级预防指南,对基线时分类为轻度缺血性卒中(NIHSS< 5)、经典TIA或非典型TIA患者进行治疗。通过面对面随访来确定中风风险(7天、90天和10年风险)和所有主要血管事件的风险,并与基础研究人群的预期风险进行比较。
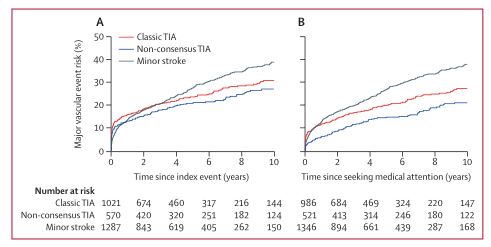
2002年4月1日至2018年3月31日期间,2878名患者被确定为轻度缺血性中风(n=1287)、典型TIA(n=1021)或非典型TIA发作(n=570)。中位随访时间为5.2年后,共发生了577例首次复发中风。
总的来说,非典型TIA发作后90天中风风险与典型TIA相似(10.6% vs 11.6),高于一过性黑蒙后卒中风险(4.3%)。然而,非典型TIA发作患者在寻求医疗帮助的可能性低于典型TIA发作患者(59% vs 75%),在寻求治疗前往往更易复发中风(8% vs 5%),风险为典型TIA患者的1.77倍。
排除此类复发性卒中后,非典型TIA患者在就诊后7天里的中风风险(2.9%)也远高于普通人203倍;对于当天就诊的非典型TIA患者,就诊后7天中风风险(5.9%)更是普通人的300倍。
此外,典型和非典型TIA患者10年主要血管事件风险相似(27.1% vs 30.9%)。房颤、卵圆孔未闭和动脉狭窄的基线患病率在典型和非典型TIA患者中也相似。然而,非典型TIA患者发生后循环狭窄的风险增加121%。
因此,与典型TIA发作相比,非典型TIA发作患者具有较高的早期和长期中风风险。将症状不典型的患者考虑入内后,TIA诊断将增加约50%。
参考文献:
Diagnosis of non-consensus transient ischaemic attacks with focal, negative, and non-progressive symptoms: population-based validation by investigation and prognosis. DOI:https://doi.org/10.1016/S0140-6736(20)31961-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
54
#研究发现#
75
#牛津大学#
71
#非典型#
77
也就是说那些非典型的症状应该引起重视
121
小卒中!!
126
#小卒中#是研究热点,需要大家关注
148
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
88
顶刊就是不一样,质量很高,内容精彩!学到很多
76