Eur J Cardiothorac Surg:胸骨深部伤口感染局部应用庆大霉素并不会缩短患者住院时间,降低死亡率
2022-06-11 MedSci原创 MedSci原创
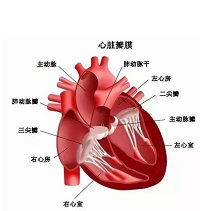
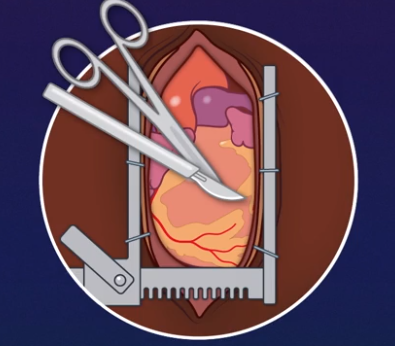
胸骨深部伤口感染(DSWI)是心脏手术的一种破坏性并发症,会导致住院时间延长和死亡率增加。在高负压Redon引流管上进行胸骨初级封闭已被证明是一种安全和可行的治疗方法。
胸骨深部伤口感染(DSWI)是心脏手术的一种破坏性并发症,会导致住院时间延长和死亡率增加。在高负压Redon引流管上进行胸骨初级封闭已被证明是一种安全和可行的治疗方法。局部应用庆大霉素可以加速伤口愈合,改善临床效果。近日,发表于Eur J Cardiothorac Surg的一项随机对照试验评估了局部庆大霉素治疗DSWI的效果。

在治疗组中,在胸骨复位时,在胸骨两半之间留置含有庆大霉素的胶原载体。在对照组中,局部没有使用抗生素。主要结果是住院时间,次要结果是死亡率、再次手术、伤口消毒时间、移除所有引流管的时间和静脉注射抗生素治疗时间。
结果,试验共纳入41名患者,其中20人被分配到治疗组,21人被分配到对照组。分析结果显示,两组的基线特征相似。治疗组和对照组患者分别在8.5天和14.5天后可以移除引流管(P值:0.343)。治疗组静脉注射抗生素的时间中位数为23.5天,对照组为38.5天(P值:0.343)。治疗组的住院时间中位数为27天,对照组为28天(P值:0.873)。治疗组的死亡率为10%,对照组为9.5%(P值:0,959)。试验研究过程中没有观察到副作用。

综上所述,这项随机对照试验表明,在治疗DSWI时加入局部庆大霉素并没有导致住院时间缩短。需要进行新的试验,以了解是否可以提前拔出引流管和缩短静脉注射抗生素治疗时间。
原始出处:
Roemer J Vos, et al., Application of local gentamicin in the treatment of deep sternal wound infection: a randomized controlled trial. Eur J Cardiothorac Surg. 2022 May 2;61(5):1135-1141. doi: 10.1093/ejcts/ezab479.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#THORAC#
88
#庆大霉素#
88
#局部#
76
#住院时间#
69
#伤口感染#
78