BMC Cancer:淋巴结检查数目(NELNs)对病理分期为 T1-3N0M0的食管鳞状细胞癌患者预后影响
2022-02-03 yd2015 MedSci原创
研究表明,淋巴结检查数目是病理分期为 T1-3N0M0的食管鳞状细胞癌患者的良好预后指标。
进行R0切除后的病理分期为 T1-3N0M0的食管鳞状细胞癌患者淋巴结检查数目(NELNs)对于术后预后的影响不明确。因此,有来自中山大学肿瘤防治中心的胸外科团队开展了相关研究,利用中肿的数据以及SEER数据库评估淋巴结数目对于该类型患者预后的影响。相关结果发表在BMC Cancer杂志上。
研究纳入中肿进行R0切除后的病理分期为 T1-3N0M0的食管鳞状细胞癌患者707例作为实验队列,而SEER数据库151例患者为验证队列。倾向评分匹配(PSM)用来匹配平衡变量,X-title软件用来计算淋巴结数目的最佳分界点。主要研究终点是总生存期(OS)。
707例患者中,男性515例(72.8%),女性192例(27.2%)。在该队列中,1年、3年和5年的总生存率分别为89.0、71.0和62.0%。在SEER队列中,1年、3年和5年的总生存率分别为56.0%、42.0%和19.0%。本中心和SEER数据库中NELNs的中位值分别为16.0 ±13.6和10.0 ±12.3。根据X-title软件基于707例患者数据计算最佳淋巴结数目为15。
研究表明,707例患者中,NELNs > 15和NELNs ≤15患者的36个月OS率为 77% vs. 65%,而60个月OS率为69% vs. 55%。NELNs > 15患者的OS明显优于NELNs ≤15患者(unadjusted HR 0.630, 95%CI, 0.506-0.784, p < 0.001)。

707例患者OS差异
462例匹配队列患者中,NELNs > 15和NELNs ≤15患者的36个月、60个月OS率分别为77% vs. 64和68% vs. 53%。NELNs > 15患者的OS明显优于NELNs ≤15患者(p= 0.0011)。
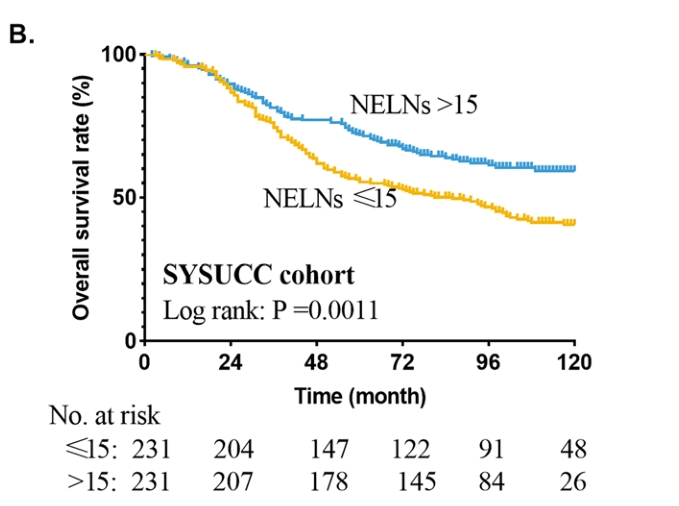
匹配462例患者OS差异
SEER数据库151例患者中,NELNs > 15患者的OS明显优于NELNs ≤15患者( p=0.044),12、36、60个月OS率分别为68% vs.50,45% vs. 41和43% vs. 29%。
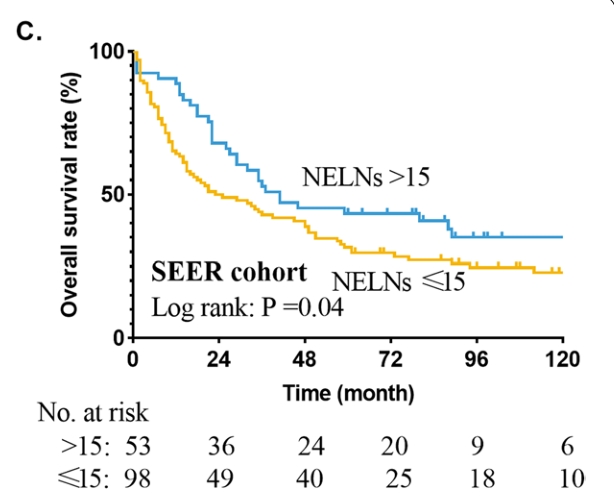
SEER数据库151例患者OS差异
两队列的多因素分析均表明 NELNs > 15可作为该类型患者的预后良好指标。
根据不同T分期进行分析时发现,T1、T2、T3患者中NELNs > 15患者的OS明显优于NELNs ≤15患者(p=0.042,p=0.007,p<0.001)。
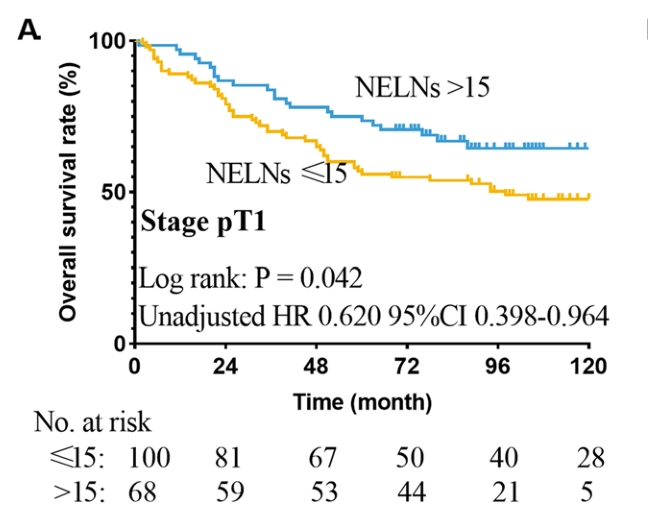
T1期患者OS差异
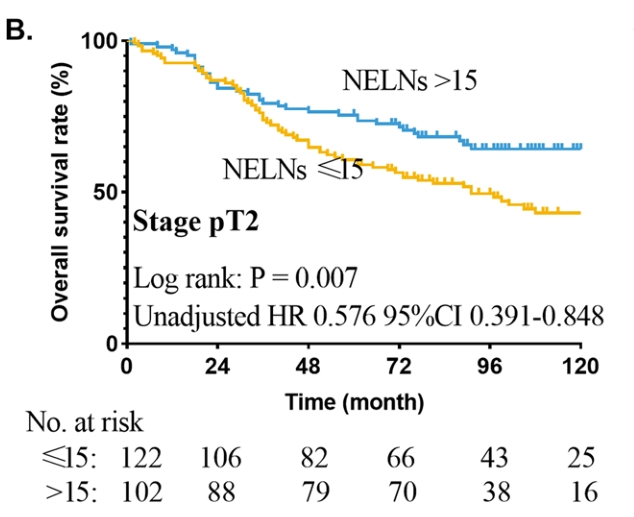
T2期患者OS差异
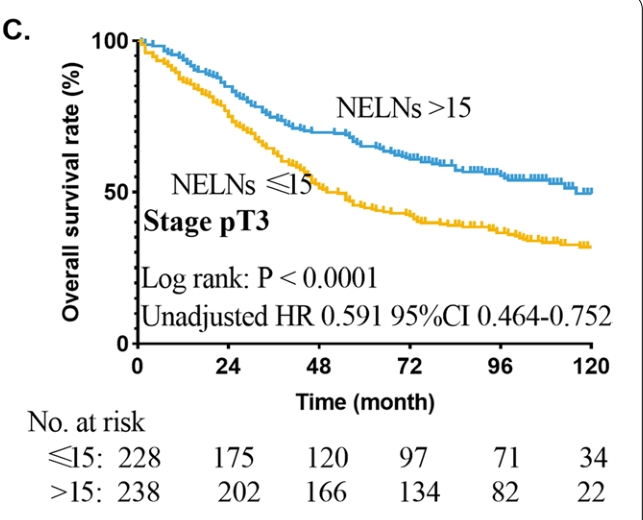
T3期患者OS差异
综上,研究表明,淋巴结检查数目是病理分期为 T1-3N0M0的食管鳞状细胞癌患者的良好预后指标。
原始出处:
Wu LL, Zhong JD, Zhu JL, Kang L, Huang YY, Lin P, Long H, Zhang LJ, Ma QL, Qiu LH, Ma GW. Postoperative survival effect of the number of examined lymph nodes on esophageal squamous cell carcinoma with pathological stage T1-3N0M0. BMC Cancer. 2022 Jan 28;22(1):118. doi: 10.1186/s12885-022-09207-x. PMID: 35090428.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞癌#
56
#患者预后#
67
#BMC#
61
#病理分期#
77
学习
78
#淋巴结#
60
#食管鳞状细胞癌#
132
#食管#
68
谢谢分享
141
学习了,谢谢分享
102