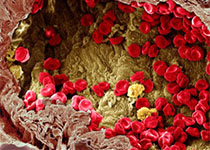
抗肿瘤免疫治疗irRC疗效评价标准详解
2018-07-10 MedSci MedSci原创
2009年国际上建议并制定肿瘤免疫治疗的疗效判断新标准—免疫相关反应标准(Immune-Related Response Criteria,irRC),以弥补RECIST或改良后的WHO标准并不完全适用于抗肿瘤细胞免疫治疗的缺陷。 irRC标准与RECIST、WHO标准的比较 RECIST与WHO标准存在的不足 以影像学资料作为疗效评价的唯一标准,以局部的疗效
2009年国际上建议并制定肿瘤免疫治疗的疗效判断新标准—免疫相关反应标准(Immune-Related Response Criteria,irRC),以弥补RECIST或改良后的WHO标准并不完全适用于抗肿瘤细胞免疫治疗的缺陷。 irRC标准与RECIST、WHO标准的比较 RECIST与WHO标准存在的不足 以影像学资料作为疗效评价的唯一标准,以局部的疗效来判定整体的治疗效果。 仅以瘤体缩小持续4周以上来评价,反映的是近期的疗效。 以单一的客观标准来来反映复杂的人体病变,忽视人的主观感受及生存时间。 irRC标准的创新之处 将可测量的新发病灶计入总肿瘤负荷中,并且将其与基线肿瘤负荷进行比较。 初次评价为irPD,在病情没有急剧恶化的情况下仍需继续治疗并进行二次评价,因为很有可能在irPD确定后4周内开始缩小,只有连续两次评价肿瘤负荷均有增加,并且大于25%才被认定为irPD。 而对于那些肿瘤负荷下降缓慢,虽然超过25%但不足50%的irSD患者,则认为他们同样属于临床获益人群。 在免疫治疗实践中发现肿瘤患者出现新的病灶并不一定提示治疗无效,相当比例的患者继续接受治疗,出现SD,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













谢谢
68
#疗效评价#
75
#评价#
68
#评价标准#
81
#irRC#
81
谢谢梅斯提供这么好的信息,学到很多
61