Spine:前路胸椎手术并发症和死亡率高
2014-07-01 lining117826 丁香园
胸椎间盘突出的发病率为1/100万。目前治疗症状性胸椎间盘突出的方法有多种。然而,手术入路大致可分为两类,前入路和非前入路。前入路的优点为手术视野开阔、脊髓损伤风险小、能最优化的减压。然而,由于前入路侵犯胸腔,这将导致肺功能障碍、疼痛和发病率增加。截止到目前,前入路和非前入路治疗胸椎间盘突出的比较研究仍未见报道。 为了比较前入路和非前入路治疗胸椎间盘突出的并发症发生率和死亡率,美国学Yosh
胸椎间盘突出的发病率为1/100万。目前治疗症状性胸椎间盘突出的方法有多种。然而,手术入路大致可分为两类,前入路和非前入路。前入路的优点为手术视野开阔、脊髓损伤风险小、能最优化的减压。然而,由于前入路侵犯胸腔,这将导致肺功能障碍、疼痛和发病率增加。截止到目前,前入路和非前入路治疗胸椎间盘突出的比较研究仍未见报道。
为了比较前入路和非前入路治疗胸椎间盘突出的并发症发生率和死亡率,美国学Yoshihara等进行了一项回顾性研究,该研究结果已在近期的Spine杂志上发表。
根据既定的纳入与排除标准,作者纳入患者25413人(数据来自美国全国住院病人样本数据库),其中前入路组5698名(22.4%),非前入路组19715名(77.6%)。患者的平均年龄分别为48.5岁和53.4岁。作者对患者的年龄、性别、种族、住院日、住院宣教、医院分区、费用等进行了分层分析。
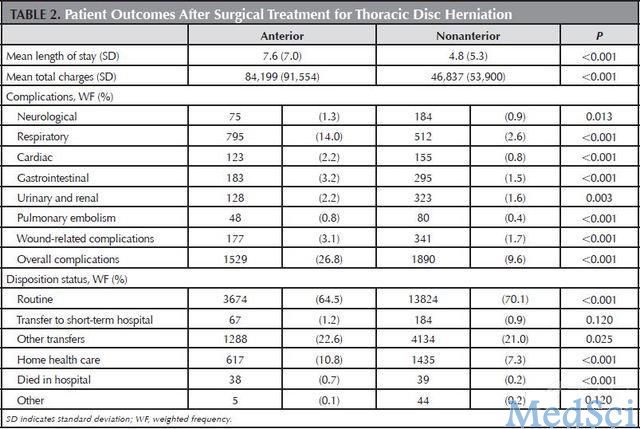
该研究结果显示,前入路术具有高的住院日(7.6 versus 4.8)、住院费用、并发症发生率(神经系统、呼吸系统、循环系统、消化系统、泌尿系统等)、和死亡率(0.7% versus 0.2%)(表1)。并且,多变量回归分析认为,高龄(大于85岁)、女性、呼吸系统/心血管系统/泌尿系统并发症为患者死亡的高危因素(表2)。

本研究的最大特点为数据来自美国全国住院病人样本数据库,纳入的研究为2000年至2009年,样本具有代表性,能反映上个年代治疗胸椎间盘突出的结果。另外,本研究发现了前入路手术具有高的并发症发生率和死亡率的特点。
然而,本研究的局限性是:1.纳入的数据可能受到样本报告的干扰,2.纳入样本为住院患者,并发症发生率和死亡率可能低估了,3.失败手术(硬件和融合)会导致住院费用增加,这一点无法明确,4.胸腔镜组样本小,无法进行分层分析。
该研究结果表明,前路胸椎间盘突出手术入路并发症发生率和死亡率更高。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#手术并发症#
0
#Spine#
61
#并发#
76
#胸椎#
71