Nat Commun:与酒精依赖性有关的离子通道
2013-12-04 Nature中文网 Nature中文网
本期Nature Communications上发表的一篇研究论文报告说,小鼠对酒精的偏好源自介导神经传输的特定离子通道发生的突变。这些发现为了解在一些形式的酒精上瘾中所涉及的不同机制提供了新见解。【原文下载】 GABA离子通道是哺乳动物神经系统正常发挥功能所必需的。以前的研究表明,酒精可能会对一些类型的GABA离子通道产生一个影响,该影响增强这些通道的活性,同时使寻找酒精的行为增加。然而,这一
本期Nature Communications上发表的一篇研究论文报告说,小鼠对酒精的偏好源自介导神经传输的特定离子通道发生的突变。这些发现为了解在一些形式的酒精上瘾中所涉及的不同机制提供了新见解。【原文下载】
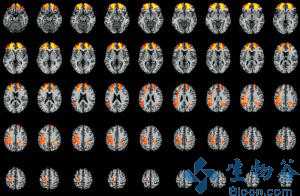
GABA离子通道是哺乳动物神经系统正常发挥功能所必需的。以前的研究表明,酒精可能会对一些类型的GABA离子通道产生一个影响,该影响增强这些通道的活性,同时使寻找酒精的行为增加。然而,这一假设一直没有被结论性地证明。为了解决这个问题,Quentin Anstee及同事研究了在一个特定类型的GABA受体上发生了突变的两种转基因小鼠。他们发现,这些小鼠表现出酒精消耗量增加和自行喝酒的行为,而且它们还具有能够自然打开的GABA通道的特点。在通道打开活动上发生的这一变化改变了小鼠大脑伏隔核(与奖赏和上瘾有很大关系的一个区域)中神经元的可激发性。
虽然这些研究是用小鼠完成的,但作者希望这些发现可以适用于人类——GABA离子通道已被发现与人类的酒精依赖性有关。如果类似发现在人类身上取得,那么它们可能会导致以一些形式的酒精依赖为目标的药物的开发。
原文出处
Anstee QM, Knapp S, Maguire EP, Hosie AM, Thomas P, Mortensen M, Bhome R, Martinez A, Walker SE, Dixon CI, Ruparelia K, Montagnese S, Kuo YT, Herlihy A, Bell JD, Robinson I, Guerrini I, McQuillin A, Fisher EM, Ungless MA, Gurling HM, Morgan MY, Brown SD, Stephens DN, Belelli D, Lambert JJ, Smart TG, Thomas HC.Mutations in the Gabrb1 gene promote alcohol consumption through increased tonic inhibition.Nat Commun. 2013 Nov 26;【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#COMMUN#
61
#Nat#
61
#酒精依赖#
71
#离子通道#
65