次全子宫切除术
(subtotal hysterectomy)
[适应证]
1.子宫肌瘤、子宫功能性出血、子宫腺肌瘤,宫颈检查正常,患者要求保留宫颈。
2.因各种原因需切除子宫,但切除宫颈有困难者。
[麻醉方法]
同子宫肌瘤剔除术。
[术前准备]
同子宫肌瘤剔除术。
[手术范围]
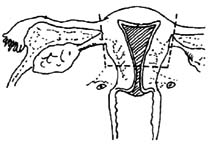
手术切除子宫体部(图1)。
 |
| 图1 次全子宫切除范围 |
[手术步骤和技术要点]
1.切口 同子宫肌瘤剔除术。
2.探查 了解子宫大小、活动度及子宫颈情况等。
 |
 |
| 图2 牵拉子宫 | 图3 处理圆韧带 |
3.切断圆韧带 钳夹两侧宫角,向腹腔外牵拉(图2)。距宫角1cm处钳夹切断圆韧带,缝扎远端(图3)。
 |
 |
| 图4 切断宫角 | 图5 宫角断端缝合 |
4.处理附件 于宫角钳夹切断卵巢固有韧带及输卵管间质部(图4),“8”字缝扎断端(图5)。
 |
 |
| 图6 打开膀胱反折腹膜 | 图7 推下膀胱 |
5.暴露子宫下段 沿子宫两侧打开阔韧带前叶及膀胱反折腹膜(图6)。提起膀胱反折腹膜,在膀胱筋膜与子宫颈筋膜间的疏松组织间隙,向下分离膀胱,达子宫峡部(图7),再沿子宫两侧剪开阔韧带后叶至子宫峡部(图8)。
 |
 |
| 图8 剪开阔韧带 | 图9 处理子宫血管 |
6.处理子宫血管 于子宫峡部水平紧贴子宫侧壁钳夹切断子宫动、静脉及宫旁组织,残端缝扎(图9)。
 |
 |
| 图10 子宫峡部环形切口 | 图11 缝合宫颈残端 |
7.切除子宫体 拉开膀胱,暴露子宫峡部,在峡部做一环形切口,贯穿宫颈管粘膜层(图10),切出子宫。宫颈残端消毒后,用可吸收线“8”字缝合(图11)。
 |
| 图12 盆腹膜缝合后 |
8.重建盆腹膜 缝合盆腔盆腹膜,将双侧附件断端、圆韧带断端、宫颈残端包埋其中(图12)。
9.关腹 分层缝合腹壁各层。
[常见失误分析]
1.出血 在处理子宫圆韧带、卵巢固有韧带、输卵管时,断端缝扎不紧或线结滑脱导致出血,故双重结扎为妥。在切断子宫动静脉时,应尽量分离子宫动静脉周围组织,认清血管,并紧贴子宫进行钳夹,牢固结扎。下推膀胱时,要分清层次,太浅或太深均会导致出血。
2.邻近脏器损伤 由于次全子宫切除手术常用于子宫与盆腔脏器粘连明显,特别是膀胱、直肠与宫颈粘连较致密时,解剖层次欠清,易出现膀胱、直肠、输尿管损伤。一旦出现应立即修补。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#全子宫切除术#
74
#切除术#
53
#子宫切除#
60
#子宫切除术#
68