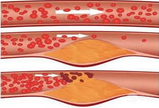
JACC子刊:冠状动脉钙化与CVD预后独立相关
2016-07-23 phylis 译 MedSci原创
目的:作者旨在确定基线冠状动脉钙化(CAC),随访CAC 及,CAC进展对心血管疾病(CVD)的影响。背景:重复CAC扫描已被提议作为跟踪总动脉粥样硬化负荷的方法。然而, CAC进展是否是未来心血管事件的预测因子尚不清楚。方法:这是一项前瞻性观察性研究,共5933名无心血管疾病患者,进行了2项检查,包括CAC评分,和随后的心血管事件的评估。用平方根法计算CAC的进展。主要终点为总体心血管事件(CV
目的:作者旨在确定基线冠状动脉钙化(CAC)、随访CAC 及CAC进展对心血管疾病(CVD)的影响。
背景:重复CAC扫描已被提议作为跟踪总动脉粥样硬化负荷的方法。然而, CAC进展是否是未来心血管事件的预测因子尚不清楚。
方法:这是一项前瞻性观察性研究,共5933名无心血管疾病患者,进行了2项检查,包括CAC评分,和随后的心血管事件的评估。用平方根法计算CAC的进展。主要终点为总体心血管事件(CVD死亡、非致死性心肌梗死、非致死性动脉粥样硬化性卒中、冠状动脉搭桥术、经皮冠状动脉介入治疗)。次要终点包括硬心血管事件、总冠心病(CHD)事件和“硬性”(hard)CHD(Hard CHD=心肌梗死+冠脉死亡)事件。
结果:基线检测2870例(48%)患者的CAC。扫描的平均时间为3.5±2。在平均随访7.3年中,第二次扫描后161例患者发生总的心血管事件。在包括基线CAC的模型中,CAC进展与总心血管事件显著相关(每间距范围HR 1.14,95%CI 1.01-1.30;),但相对于基线CAC,CAC进展的贡献相对较小(4.16 vs. 65.92)。此外,随访CAC的模型代替CAC的模型中,CAC进展与总体心血管事件不相关(HR 1.05,95%CI 0.92-1.21)。仅包括随访CAC的模型的结果,与包括基线CAC和CAC进展的模型的结果是一致的。
结论:尽管CAC进展与CVD预后独立相关,当将随访CAC包括在模型中后,这种相关性就不再显著。这些结果意味着,如果采用系列CAC扫描,最新的扫描就可以用来进行风险评估,并在这方面,CAC进展不会提供更多的预后信息。
原始出处:
Radford NB, DeFina LF, et al. Progression of CAC Score and Risk of Incident CVD. JACC Cardiovasc Imaging. 2016 Jun 23.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
69
#冠状动脉钙#
53
#动脉钙化#
56
文章很好值得关注
96
#冠状动脉钙化#
58
#ACC#
46