Cell Host Microbe:科学家阐明驱动肠道菌群失衡及炎症发生的分子机制
2017-02-10 生物谷 生物谷
图片来源:medicalxpress.com 2017年2月9日 讯 /生物谷BIOON/ --日前,一项刊登在国际杂志Cell Host & Microbe上的研究报告中,来自德州大学西南医学中心(UT Southwestern Medical Center)的科学家通过研究揭开了在炎性疾病发病过程中干扰肠道细菌平衡背后的分子途径。 研究者Sebastian Winter教授指

图片来源:medicalxpress.com
2017年2月9日 讯 /生物谷BIOON/ --日前,一项刊登在国际杂志Cell Host & Microbe上的研究报告中,来自德州大学西南医学中心(UT Southwestern Medical Center)的科学家通过研究揭开了在炎性疾病发病过程中干扰肠道细菌平衡背后的分子途径。
研究者Sebastian Winter教授指出,深入理解这些途径或许能够帮助我们开发预防或治疗多种疾病的新型策略,比如炎性肠病(IBD)、特定的胃肠道感染以及结直肠癌等。目前在美国有超过100万人都患有炎性肠病,炎性肠病是一种慢性、长期的肠道炎性疾病,目前并没有有效的治疗和预防措施。
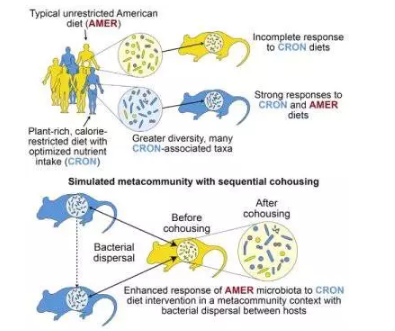
本文研究中研究人员就解释了肠道炎性发生期间肠道改变背后存在的关键机制,研究者表示,肠道炎症和肠道从细菌中获取的营养物质的改变直接相关,健康人的肠道中聚集着多种微生物群落,肠道细菌细胞的数量大约是人体细胞数量的10倍,在一个人一生的大部分时间里,机体的微生物群落都会帮助促进消化,保护机体免于感染或者调节机体健康免疫系统的发育。
在炎性肠病、胃肠道感染以及癌症发过程中会伴随肠道炎性的发作,同时肠道微生物群落的组分也会被完全干扰,有益细菌的数量会开始慢慢减少,有些甚至会变成有害细菌,因此肠道微生物群落的失衡被认为会加速肠道炎性的过程。健康的肠道通常是缺乏氧气的,而有益细菌也会非常适应这些低氧的环境,并且通过发酵来破碎食物中的纤维,而有害细菌,比如大肠杆菌,并不会像有益细菌那样,其往往会在高水平氧气的环境中“茁壮生长”。
研究者Winter解释道,炎性会改变环境,进而就会干扰肠道中栖息的厌氧菌的生长,但大肠杆菌往往偏爱这种环境,其往往会等待一次“偶然事件”发生来开始发起攻势,比如机体炎症发生等。在炎症发生过程中,氧气可用性的增加会帮助大肠杆菌在炎性肠道中生存。通过进行呼吸作用,有益细菌所产生的大量废弃物会被肠道中的大肠杆菌再度循环利用,而大肠杆菌会将这些代谢废物变废为宝,并且促进大肠杆菌群体快速生长扩张。
阐明肠道菌群失衡的分子机制或为后期科学家们开发新型疗法和诊断策略非常重要,当然研究人员也希望能够开发出更加有效的策略来治疗炎性肠病以及炎性相关的结直肠癌,比如开发一种新型药物来抑制大肠杆菌的特殊代谢功能。最后研究者Winter说道,如果我们通过有益的共生细菌来干扰废弃物的产生,这样我们就能阻碍有害细菌(比如大肠杆菌)的代谢,进而就会影响有害细菌的生长,从而就能保护整个肠道微生物群落系统的平衡。目前最有效的策略或许就是抑制肠道中共生的大肠杆菌的特殊代谢作用来避免其快速繁殖以及对机体肠道产生副作用。(生物谷Bioon.com)
本文系生物谷原创编译整理,欢迎转发,转载需授权!点击 获取授权 。更多资讯请下载生物谷 APP.
原始出处:
Elizabeth R. Hughes, Maria G. Winter, Breck A. Duerkop, et al. Microbial Respiration and Formate Oxidation as Metabolic Signatures of Inflammation-Associated Dysbiosis. Cell Host & Microbe. (2017)













#Cell#
64
#CEL#
119
#CRO#
67
#Micro#
64
#肠道菌#
80