本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2017-03-23 Leo.C MedSci原创
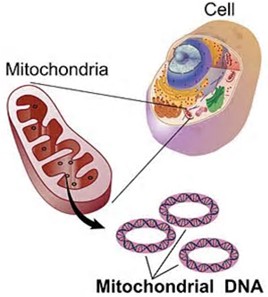
线粒体蛋白调节脂代谢抑制乳腺癌细胞增殖

掉发是癌症治疗过程中最严重的副作用之一。而科学家们早在80年代就指出通过冷却患者的头皮,能够有效避免化疗过程中头发掉落的问题。2015年,一种叫做DigniCap的冷却设备被FDA批准用于女性乳腺癌治疗的过程中。
近些年女性患乳腺癌的几率越来越高,也许跟现代女性工作压力、生活压力导致的生活习惯的改变等都有一定关系。2016年10月,发表在《J Natl Cancer Inst.》的一篇3项前瞻性研究和已发表研究的荟萃分析调查了值夜班对乳腺癌发病率的影响。
曲妥珠单抗可显着提高 HER-2 阳性乳腺癌患者的总生存期(OS)和无病生存期(DFS),但目前尚无相关长期随访数据。
专家说:“许多女性可以通过一种新型的乳腺癌药物来帮助生物治疗,目前只能作为临床试验的一部分。但是,在不久的将来有很大的希望被用于单独治疗乳腺癌”。专家估计,多达五分之一的患者可能受益。科学家说:“英国每年约有 10,000 名妇女可能受益于新型乳腺癌治疗”。生物治疗可以帮助抵抗罕见的遗传错误导致的乳腺癌,如 BRCA 一个女演员安吉丽娜·朱莉携带了一种罕见的遗传错误基因,从而患有一种区别于
四分之三的乳腺癌肿瘤由雌性激素驱动。这些肿瘤经常用药物治疗以抑制雌激素受体活性,但不幸的是,至少一半的患者对这些治疗没有反应,使它们成为耐药性肿瘤。 现在,来自斯克里普斯研究所(TSRI),加利福尼亚大学(UC),圣地亚哥和伊利诺伊大学的佛罗里达州校园的科学家发现两种免疫系统分子可能是雌激素,驱动乳腺癌。研究人员认为,这一发现可能为成千上万患有雌激素驱动的乳腺癌的患者开创了
目前,关于高血压与乳腺癌风险之间相关性的研究存在一定的矛盾。近期,一项发表在杂志Sci Rep上的研究进行了系统评价和荟萃分析,总结了有关高血压与乳腺癌风险之间的相关证据。通过对PubMed、EMBASE和Cochrane图书馆的综合文献检索,确定截至2016年8月的相关合格研究。此项荟萃分析包括报告了相对风险(RR)与相应95%置信区间(CI)的观察性研究。通过使用随机效应模型汇集个人研究结果。


梅斯医学MedSci APP
医路相伴,成就大医
#癌细胞增殖#
61
#Nat#
56
#癌细胞#
65
#细胞增殖#
58
#脂代谢#
67