单纯主动脉瓣反流TAVI治疗的现状及挑战
2020-11-30 《门诊》杂志 门诊新视野
长久以来,主动脉瓣反流的治疗本身是一个难题,无论采取外科手术治疗或TAVI都没有足够的临床循证依据证明其有效性与安全性。
单纯性主动脉瓣反流(AR)的TAVI治疗是TAVI技术延伸应用的困难领域,此类患者往往非钙化性主动脉狭窄(Non Calcific AS)与AR共存,临床处理颇为棘手,TAVI过程中瓣膜的选择及锚定至关重要。瓣膜的准确定位颇具挑战性,有些瓣膜较硬,容易滑动并可能造成封堵不全;采用瓣中瓣(VALVE-IN-VALVE)技术虽也能解决反流问题,但目前缺乏长期随访结果,远期预后皆待考量。2020年11月22日,在成都国际心脏瓣膜疾病介入治疗会议(PCR-CIT CHINA CHENGDU VALVES)上,来自法国波尔多里尔大学附属医院Thomas MODINE教授,阐述了单纯主动脉瓣反流TAVI治疗的现状与面临的挑战。
TAVI能否用于单纯性AR?
严重主动脉瓣反流患者的临床预后不佳,在没有得到良好治疗的情况下,死亡风险高达10~20%。目前,经外科主动脉瓣置换术(SAVR)仍是单纯性AR临床治疗的基石,但其临床获益不佳。根据欧洲心脏病流行病学数据报告,在经外科主动脉瓣置换术(SAVR)治疗的单纯性AR患者人群中,仅有21.8%的患者LVEF(左室射血分数)达到30~50%,2.7%的患者LVEF低于30%。TAVI技术处于蓬勃发展阶段且前景光明,因此,临床医师正努力尝试将TAVI技术用于单纯性主动脉瓣反流的治疗,多个相关临床随机试验正在开展。
应用于单纯性AR的新型瓣膜
随着瓣膜技术的不断发展,一些新型设计如可固定到自身瓣膜的“钳夹”,可为无钙化主动脉瓣病变提供一个非常重要的解决方案,使得TAVR有效治疗单纯性AR成为可能。虽然目前临床病例有限,但已有多种瓣膜应用于单纯性AR的TAVI治疗。
JENAVALVE TA(图1)、J-Valve(图2)两者都是自膨胀式瓣膜,JENAVALVE TA具有径向支撑力强的特点,其支撑效果良好但并未广泛应用;J-Valve应用更为普遍且获益良好,可能成为未来治疗方案的常规选择。除此之外,ACURATE TA VALVE瓣膜具有良好的锚定功能。同时,更多具有不同特色及适应性的瓣膜正在进一步开发。
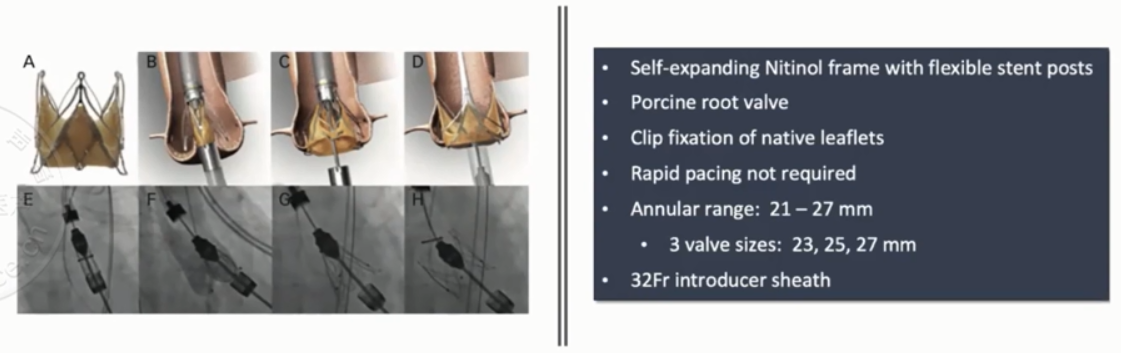
图1. JENAVALVE TA瓣膜
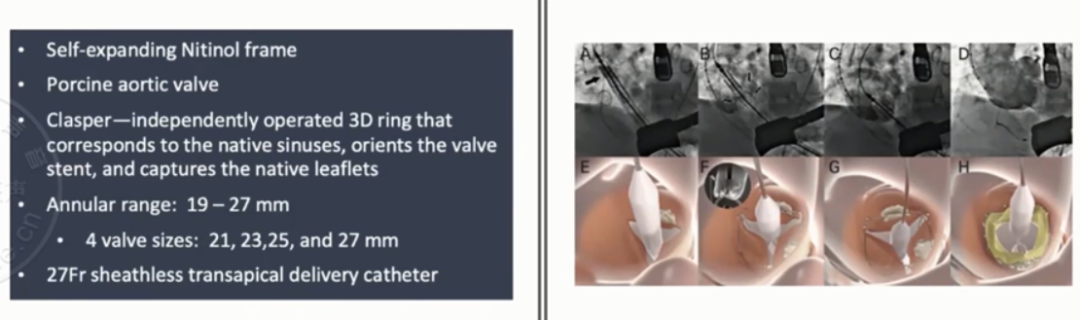
图2. J-Valve瓣膜
单纯性AR TAVI治疗面临挑战
目前,单纯性AR的TAVI治疗依旧面临众多挑战,术后并发症是主要方面,如瓣膜移位、瓣周漏(PVL)、传导阻滞等。单纯性AR患者若合并轻到中度的AS,瓣叶及瓣环大多会有增厚且质地变韧,甚至轻度钙化等表现,更有利于瓣膜的稳固锚定,相较于合并高度AS患者,出现瓣周漏的机会也更小,为TAVI治疗的可行性提供了保障。
现有关于单纯性AR的TAVI治疗的临床研究数据多来自于单中心、小样本研究,尽管这些研究的部分报道认为单纯性AR在经TAVI治疗后临床获益显着,但一项来自日本的最新的META分析研究结果却不尽如人意(图3)。该荟萃分析纳入了至今所有TAVR应用于单纯性AR治疗的各类型瓣膜病例共911例,主要结果提示:器械成功率不高(84%~96.3%),转外科手术比例高且PVL的发生率远高于预期;再行瓣中瓣手术治疗达4.7%,永久起搏器植入比例也高达8.3%。因此,单纯性AR的TAVI治疗为患者带来的临床获益仍未可知,如何更有效、更规范化地实施TAVI以提高其临床疗效,仍待进一步的临床经验总结及未来更多RCT研究提供可循依据。
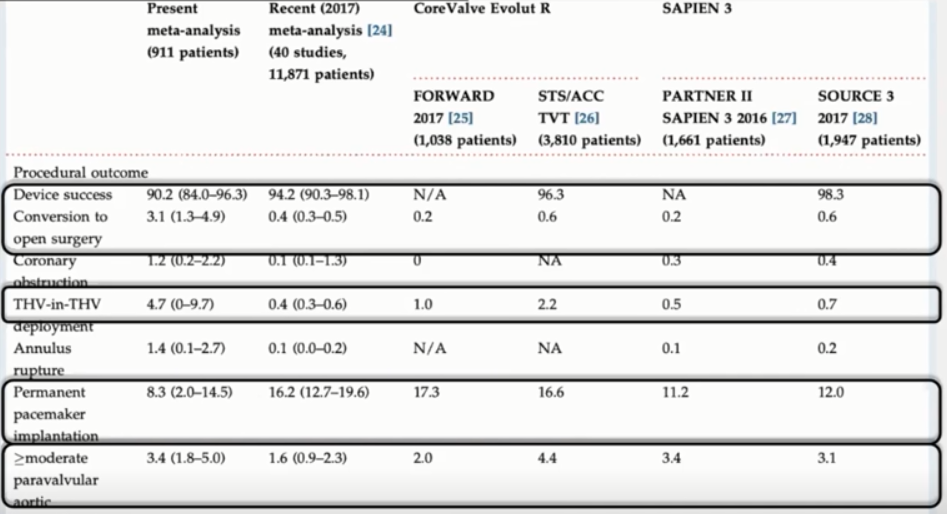
图3. 日本最新Meta数据分析结果
近期,国际ISO发布了针对单纯性主动脉瓣反流TAVI治疗的相关标准(ISO 5840-3),给出的系列建议主要涉及以下几方面:
1.单纯性主动脉瓣反流与主动脉瓣狭窄解剖结构特征存在明显差异,主动脉瓣狭窄通常以钙化病变为主,单纯性AR则不然,临床医生诊疗需建立在对两者解剖结构理解的基础之上;
2.在针对单纯性AR进行TAVI治疗时,应密切关注PVL是否发生与PVL的程度;
3.进行瓣膜选择时,应综合考量瓣膜的解剖结构、径向支撑力、外围包裹力量是否充足;
4.进行瓣膜的锚定亦十分关键,通常选择面积较大的瓣膜,以预防瓣膜滑落;
5.瓣膜的持久性亦是影响TAVI临床效果的重要因素。
相信在最新标准的指导下,进一步开展单纯性AR的TAVI治疗相关大型临床RCT研究将有迹可循;未来的挑战不仅在于技术本身的进一步规范和优化,更在于现代科技大背景下器械的更新迭代以及术者临床思维的创新与手术技巧的飞跃。
总 结
长久以来,主动脉瓣反流的治疗本身是一个难题,无论采取外科手术治疗或TAVI都没有足够的临床循证依据证明其有效性与安全性。而单纯性AR患者常合并非钙化性主动脉瓣狭窄,由于其病理因素特殊性以及病变结构的多样化,针对此类患者TAVI治疗的发展历程更可谓步履维艰。振奋人心的是,TAVI领域的专家始终坚信TAVI技术的不断进步可为单纯性AR治疗提供全新的出路,近年来一些相关研究结果亦初步提示,TAVI治疗单纯性AR的可行性与有效性。尽管TAVI治疗单纯性AR之路仍十分漫长,但已不再是一片“盲区”,广大心血管医师应在已有经验的基础上不断积累、分析总结、凝练提升,走出思维定式,勇于向面临的挑战发难。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#主动脉瓣反流#
82
#主动脉瓣#
67
#主动脉#
75
#反流#
92