质子泵抑制剂可导致肾衰竭?
2015-04-21 小闪 cmt
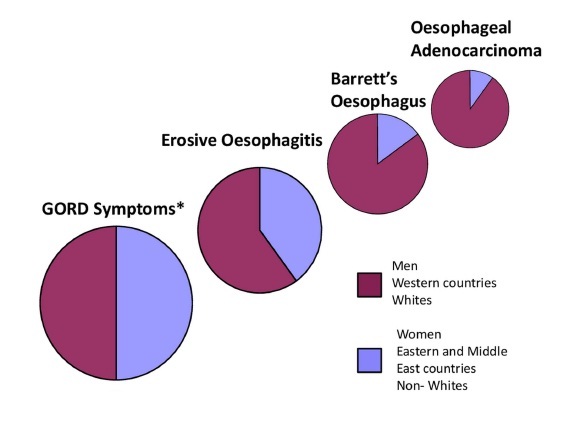
研究发现,老年患者服用质子泵抑制剂,一种治疗胃灼热和反酸一种常见的药,导致肾衰竭住院率的可能性是未服用者的两倍。虽然副作用是极其罕见的,但是相关性是令人担忧的,因为每年数百万人服用这些处方药和非处方药的销售的药物,包括奥美拉唑,兰索拉唑和奥美拉唑口服混悬液。“一般来说,这些药物耐受性很好,服用这些药物的绝大多数患者不会发展(肾功能衰竭)或其他严重的问题,”研究的首席作者Tony Antoniou,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#质子泵#
74
厉害啊!
144
这么厉害?
158
#抑制剂#
71
有待观察
135
不知道
141
#肾衰竭#
73
有没有对比过两组患者基线时合并症的差异,服用PPI的人,也许是因为其他疾病的胃肠道表现,或许是服用其他药物后的胃肠道不适,如果基线没有可比性,这个结论也没有意义。最近怎么对PPI有种妖魔化的倾向了?
171
不会吧
141