Neurology:患有多发性硬化症的妇女患围产期抑郁症的风险增加
2021-04-30 Freeman MedSci原创
Neurology:患有多发性硬化症的妇女患围产期抑郁症的风险增加

对于患有多发性硬化症的妇女在围产期发生抑郁症和焦虑症的情况,目前了解有限。一项研究发现,患有多发性硬化的父母中,26%伴有怀孕相关的抑郁症或焦虑症,而在没有多发性硬化症的父母中,这一比例只有19%。
母亲的精神病合并症影响儿童的心理健康和发展的脆弱性。由于患有多发性硬化症的母亲患抑郁症和焦虑症的风险增加,因此在围产期确定与这些症状相关的风险因素很重要,因为这有利于给有风险的妇女提供最佳的预防、治疗和跟踪。
我们的主要目的是调查怀孕期间和产后6个月抑郁症和焦虑症的发生情况。我们研究了1)有既定多发性硬化症诊断的妇女,2)有多发性硬化症症状但尚未得到诊断的妇女,以及3)在产后几个月或几年内有临床多发性硬化症症状的妇女。后两组被包括在内,因为她们在围产期可能有多发性硬化症的亚临床或前驱表现。我们的次要目的是调查与多发性硬化症有关的因素和社会心理方面在多大程度上影响了这些症状的发生。
藉此,挪威University of Bergen的Karine Eid等人,对114,629名孕妇被进行探究,他们加入了1999-2008年的挪威母亲、父亲和儿童队列研究中。
通过调查问卷评估了怀孕期间和怀孕后的抑郁症和焦虑症。患有多发性硬化症的妇女从国家健康登记处和医院记录中确定,并分为:
1)怀孕前诊断的多发性硬化症(n = 140),怀孕后诊断的多发性硬化症。
2)怀孕前发病的症状(n = 98)
3)怀孕后发病的症状(n = 308)
35名妇女在产后被诊断为MS。
参考组(n = 111,627)由没有多发性硬化症的妇女组成。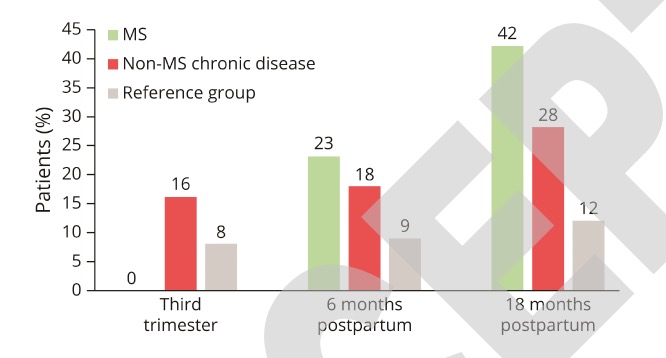
他们发现,怀孕前被诊断为多发性硬化症的妇女,在怀孕三个月内患抑郁症的调整后的几率为2.0(95%置信区间为1.2-3.1)。
风险因素包括:不利的社会经济因素、精神疾病史和身体/性虐待。焦虑的风险没有增加。
在产后被诊断为多发性硬化症的妇女,患产后抑郁症的风险特别高。怀孕后5年内出现多发性硬化症症状的妇女,在怀孕期间抑郁症和焦虑症的风险都增加了,而在症状出现后5年以上的妇女则没有。
这个研究的重要意义在于,发现了:患有多发性硬化症的妇女患围产期抑郁症的风险增加。怀孕后5年内出现多发性硬化症症状的妇女在怀孕期间患抑郁症和焦虑症的风险也会增加。
原文出处:
Perinatal Depression and Anxiety in Women with Multiple Sclerosis: A Population-Based Cohort Study
Karine Eid, Øivind Fredvik Torkildsen, Jan Aarseth, Heidi Øyen Flemmen, Trygve Holmøy, Åslaug Rudjord Lorentzen, Kjell-Morten Myhr, Trond Riise, Cecilia Simonsen, Cecilie Fredvik Torkildsen, Stig Wergeland, Johannes Sverre Willumsen, Nina Øksendal, Nils Erik Gilhus, Marte-Helene Bjørk
Neurology Apr 2021, 10.1212/WNL.0000000000012062; DOI: 10.1212/WNL.0000000000012062
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#围产期抑郁症#
61
#围产期抑郁#
0
#多发性#
63
值得学习
92
#硬化症#
74
#Neurol#
50