6个月未查出病因 竟是罕见心脏肿瘤
2017-11-25 陈旭岩 王仲 急诊临床病案评析:感染与心血管性疾病
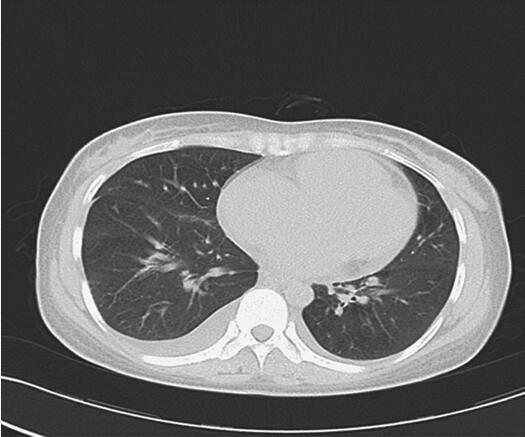
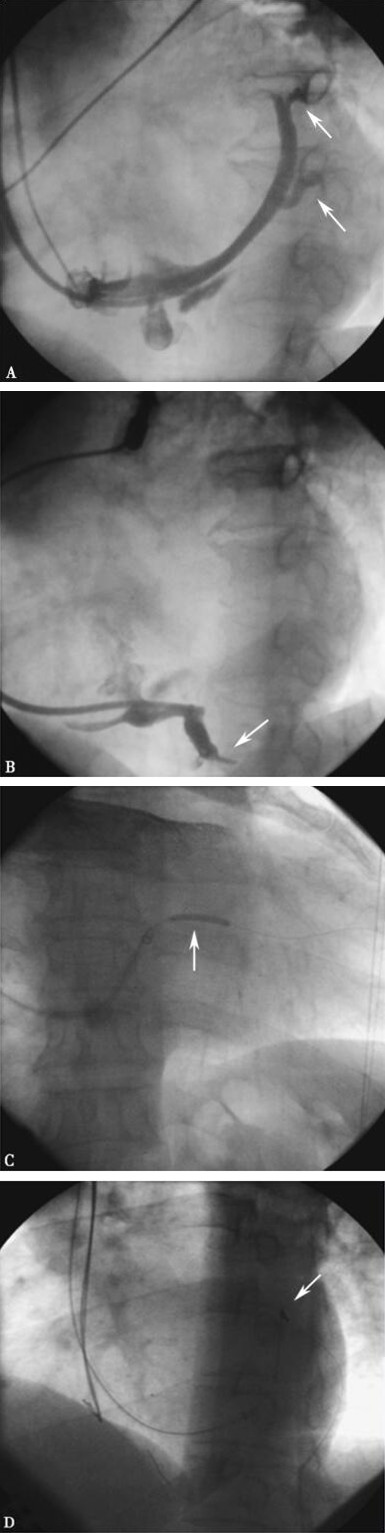
32岁女性患者入院前6个月出现阵发性咳嗽、气喘,曾予以支气管炎药物但未缓解。收治入院后,初步诊断风湿性心脏病可能性大。后经心脏彩超和专家会诊,最终确诊为左心房恶性纤维组织细胞瘤。该病例系心脏原发肿瘤,实属罕见,术前不易确诊,因此患者病情延误,手术时已进展为恶性。内科医师需开拓临床思维,重视体格检查,减少漏诊及误诊以避免悲剧的发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习到了!!谢谢!!
78
#心脏肿瘤#
57
学习一下谢谢
95
#罕见#
83
学习一下谢谢
83
学习
87
学习了受益匪浅
74
学习
62