Cancer Discov & Clin Cancer Res :年龄是黑素瘤治疗耐药性的主要决定因素
2020-11-03 MedSci原创 MedSci原创
约翰霍普金斯大学研究揭示了衰老导致黑色素瘤扩散和治疗耐药性的的新机制。
癌症一直被认为是一种衰老性疾病,60%的发病和70%的死亡发生在65岁以上的人身上。近日,由约翰霍普金斯大学基梅尔癌症中心和约翰霍普金斯大学彭博公共卫生学院的研究人员发表在Cancer Discovery 和Clinical Cancer Research上的新发现揭示了衰老导致黑色素瘤扩散和治疗耐药性的的新机制。


研究人员报告说,老年成纤维细胞持续上调脂肪酸转运蛋白FATP2,并增加了肿瘤内及周围微环境中脂肪酸的摄取。当接触到抗癌药物时,与老化成纤维细胞一起培养的黑色素瘤细胞会抵抗细胞死亡,但在与年轻成纤维细胞一起培养的细胞中很少发生这种情况。“在治疗过程中摄入大量脂肪可以保护黑色素瘤细胞。”研究人员指出。
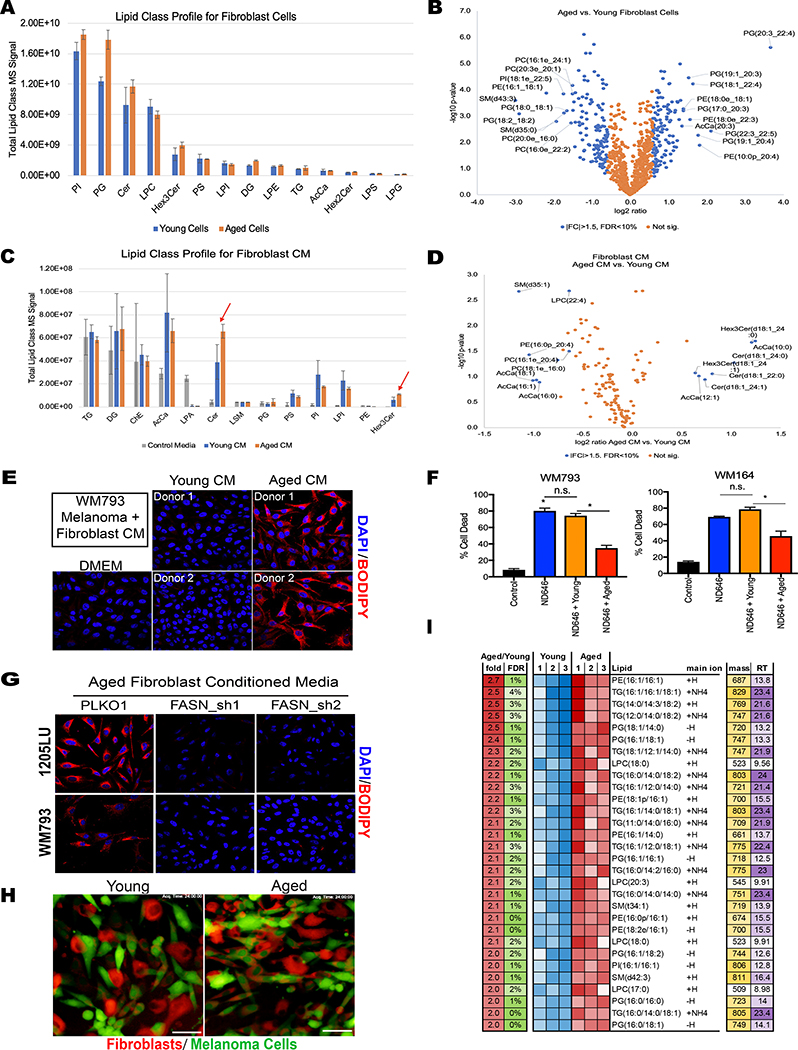
当暴露于老化的成纤维细胞中时,黑色素瘤细胞显示出较高的脂质水平。
这一发现建立在2016年Nature杂志的一项研究上,该研究报告了一种黑色素瘤小鼠模型,在该模型中,促癌基因BRAF、PTEN和CDKN2A被删除,从而容易长出肿瘤。研究发现,癌症在6到8周大的年轻老鼠的皮肤上生长得更好,但是在1岁或更大的老鼠身上更容易从皮肤转移到肺部。利用药物抑制BRAF癌基因是临床上治疗黑色素瘤的一种靶向治疗方法。在2016年的研究中,Weeraratna的实验室显示,靶向BRAF癌基因在降低老年小鼠的肿瘤生长方面效果较差,一项关于患者对BRAF抑制剂反应的研究证实了实验室的研究结果,显示完全反应最常发生在55岁以下的患者身上。
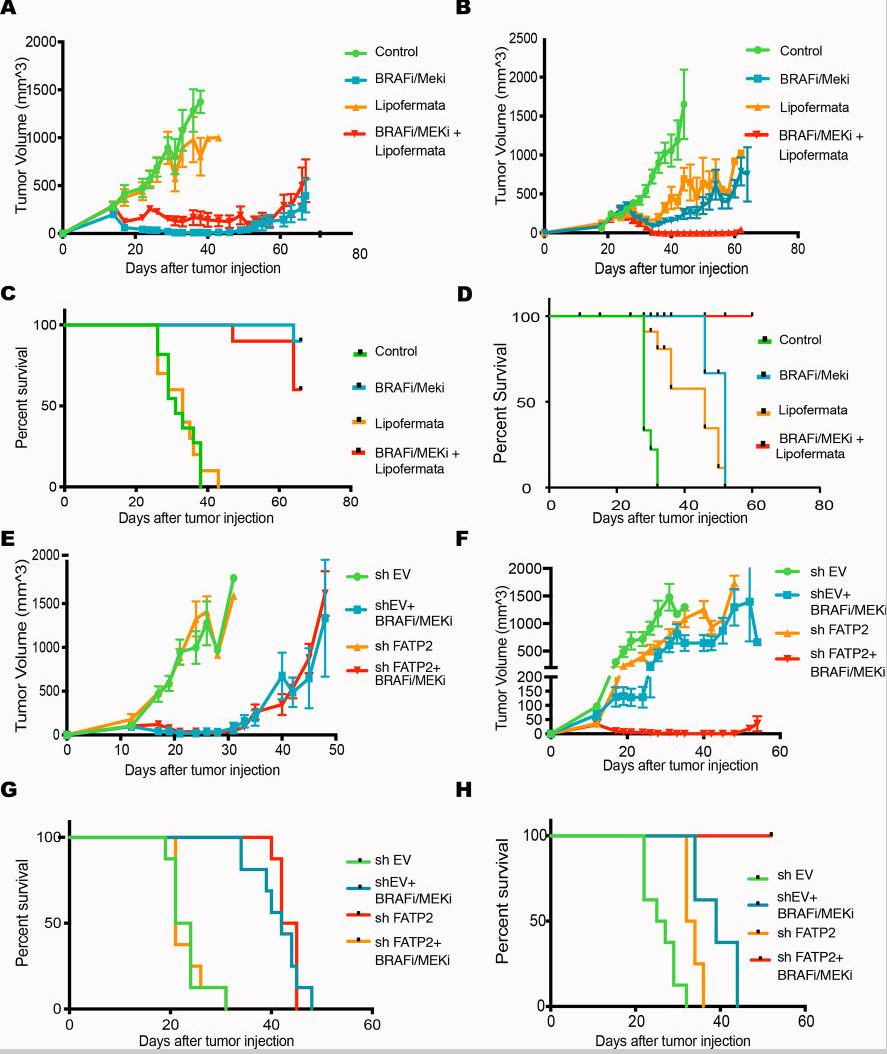
在当前的研究中,Weeraratna博士和合作者使用了该途径的新一代抑制剂,包括针对BRAF途径两个分支的药物,并评估了同时消耗FATP2的影响。
研究人员报告说,在老年小鼠中,BRAF靶向治疗最初起作用,减少了肿瘤体积,但肿瘤在10到15天内又复发了。然而,当他们在靶向治疗中加入一种FATP2抑制剂时,肿瘤在60天内消失了,没有复发。
“年龄是最明显的因素,”研究者指出。“在年轻的模型中,黑色素瘤细胞最初对靶向治疗有反应,针对FATP2没有进一步的影响。在老年模型中,靶向治疗对黑素瘤细胞没有反应,当FATP2被耗尽时,肿瘤大小完全退化,并且超过两个月(在小鼠实验中是相当长的一段时间)后才开始生长。”
这是一个至关重要的发现,因为大多数癌症研究动物模型都是使用的年轻老鼠,这可能会掩盖年龄相关的因素。
Weeraratna博士说:“因为我们使用的是基因成分相同的小鼠模型,这些研究指出了周围正常细胞的关键作用,并告诉我们不仅仅是基因在驱动癌症。” 下一步是开发一种FATP2抑制剂,一旦证明是有效的,可以与靶向治疗相结合来改善治疗效果,特别是对老年患者。
体内抑制FATP2可增强BRAF和MEK联合治疗
在另一篇发表在Clinical Cancer Research研究中,Weeraratna、Mitchell Fane博士及其同事评估了患者对抗血管生成药物Avastin的反应。(血管生成指的是滋养肿瘤的血液供应,并促进癌细胞转移到身体其他部位。抗血管生成药物,如Avastin,通过切断血液供应中的癌症而起作用。)
研究人员使用了之前英国一项对1343名术后接受Avastin治疗的黑素瘤患者的研究数据,将患者对药物的反应按年龄进行分解。理论上血管生成随着年龄的增长而增加,所以Weeraratna博士认为在治疗中老年患者会比年轻患者获益更多,但事实恰恰相反。结果显示年龄在45岁及以上的患者实际上没有受益于Avastin,相反,年龄在45岁以下的患者确有更长的无进展生存期。
Avastin通过阻断血管生成促进基因VEGF发挥作用,因此Weeraratna博士和他的团队研究了癌症基因组图谱数据库中年龄分层的黑色素瘤样本,以了解VEGF在年轻和老年患者中扮演的角色,并找到解释为什么Avastin对老年患者无效的线索。研究人员发现,在老年患者中,VEGF及其相关受体的表达均显著降低。相反,他们发现另一种蛋白质,sFRP2,在55岁以上的病人中,是促进血管生成的主要原因。
他们的发现得到了老鼠模型研究的支持。当研究人员给小鼠一种抗VEGF抗体时,它减少了近50%的新血管的生长,但是当同时给予sFRP2蛋白时,抗VEGF抗体没有效果,这证实了sFRP2是另一种血管生成的驱动因素。研究人员计划未来将进一步研究阻断sFRP2的抗体,作为55岁以上对阿瓦斯丁无反应的患者的潜在治疗方法。
最后,Weeraratna博士指出,这两项研究都清楚地表明,在开展实验和临床试验时,年龄是一个必须考虑的参数。
参考文献:1. Gretchen M. Alicea, et al. Changes in Aged Fibroblast Lipid Metabolism Induce Age-Dependent Melanoma Cell Resistance to Targeted Therapy via the Fatty Acid Transporter FATP2. Cancer Discovery, 2020; 10 (9): 1282 DOI: 10.1158/2159-8290.CD-20-0329
2. Mitchell E. Fane, et al. sFRP2 Supersedes VEGF as an Age-related Driver of Angiogenesis in Melanoma, Affecting Response to Anti-VEGF Therapy in Older Patients. Clinical Cancer Research, 2020; 26 (21): 5709 DOI: 10.1158/1078-0432.CCR-20-0446
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了
64
#决定因素#
72
#Dis#
62
学习了
98
#黑素瘤#
75
#ISC#
44
年龄,这个因素很关键
113