Eur Respir J:体力活动、久坐与阻塞性睡眠呼吸暂停发生率的关系
2021-07-27 MedSci原创 MedSci原创
较高水平的体力活动和久坐时间缩短与较低的OSA发病率相关。代谢因素在久坐行为和OSA发病率之间相关性中的潜在介导作用可能取决于久坐行为的类型。该研究的结果表明,积极的生活方式可能会降低OSA的发病率。
体力活动减少和久坐可能通过增加肥胖、炎症、胰岛素抵抗和体液潴留而促进阻塞性睡眠呼吸暂停(OSA)的发生发展。然而,流行病学证据仍然很少,且主要限于横断面研究。

近日,呼吸疾病领域权威杂志Eur Respir J上发表了一篇研究文章,研究人员前瞻性地随访了来自护士健康研究(2002-2012)的50332名女性、来自护士健康研究II(1995-2013)的68265名女性和来自卫生专业人员随访研究(1996-2012年)的19320名男性。每2-4年通过问卷调查评估休闲体力活动(通过任务[MET]小时/周的代谢当量来评估)和坐着看电视和工作/离家的时间。医生诊断的OSA由经过验证的自我报告来确定。Cox模型用于估计与身体活动和久坐行为相关的OSA发病率的风险比(HR)和95%置信区间(CI)。
在2004663人次每年的随访期间,研究人员记录了8733例OSA事件。在对潜在混杂因素进行调整后,体力活动MET≥36.0小时/周与<6.0MET小时/周受试者相比OSA的合并HR为0.46(95%CI为0.43-0.50;趋势p<0.001)。
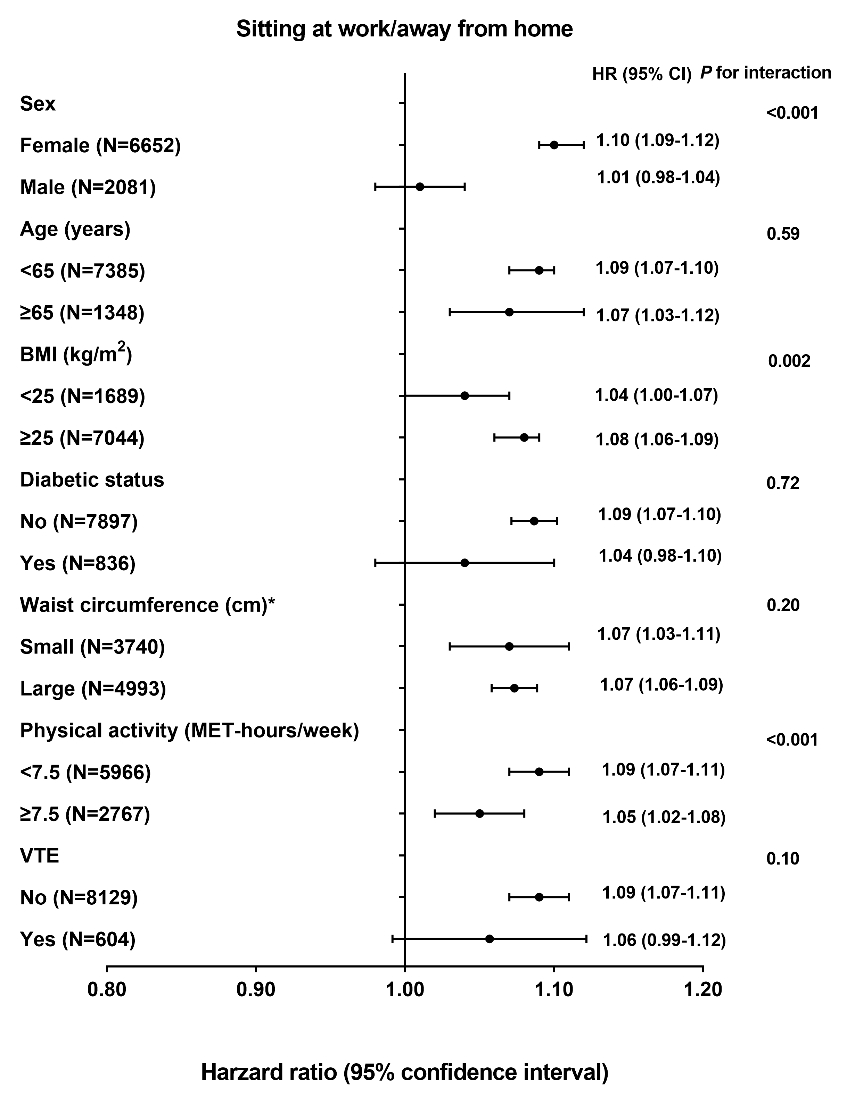
与看电视<4.0h/周的参与者相比,看电视时间≥28.0h/周的参与者发生OSA的多变量调整HR(95%CI)为1.78(1.60-1.98)(趋势p<0.001)。对包括BMI和腰围在内的几个代谢因素进行额外调整后,看电视的时间与发生OSA的关联之间不再具有统计学显著性(趋势p=0.18)。
由此可见,较高水平的体力活动和久坐时间缩短与较低的OSA发病率相关。代谢因素在久坐行为和OSA发病率之间相关性中的潜在介导作用可能取决于久坐行为的类型。该研究的结果表明,积极的生活方式可能会降低OSA的发病率。
原始出处:
Yue Liu,et al.Physical activity, sedentary behavior, and incidence of obstructive sleep apnea in three prospective US cohorts.Eur Respir J.2021.https://erj.ersjournals.com/content/early/2021/06/17/13993003.00606-2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阻塞#
102
#发生率#
93
#睡眠呼吸#
85
#呼吸暂停#
79