JAMA Oncol:卡培他滨维持治疗可明显改善转移性鼻咽癌患者的生存预后
2022-02-20 xiaozeng MedSci原创
卡培他滨维持治疗可显著延长经含卡培他滨方案诱导化疗后获得疾病控制的转移性鼻咽癌患者的无事件生存期
卡培他滨维持治疗可改善各种类型癌症患者的生存预后,但有关卡培他滨维持治疗在转移性鼻咽癌 (NPC) 中的疗效和安全性的数据有限。
本研究旨在评估卡培他滨维持治疗在转移性鼻咽癌中的疗效和安全性。
这是一项在我国中山大学癌症中心开展的随机3期临床试验,在2015年5月16日至2020年1月9日期间,共招募了104位新确诊的转移性鼻咽癌患者,这些患者经紫杉醇、顺铂、卡培他滨诱导化疗(4-6个疗程)后获得了疾病控制。受试患者被1:1双随机分成了两组,接受卡培他滨维持治疗(1000 mg/m2,2/日,口服,吃两周停一周)+最佳的支持治疗(BSC)或仅接受BSC。主要终点是无进展生存期(PFS)。次要终点是客观缓解率、缓解持续时间、总生存期和安全性。
两组患者的PFS和缓解持续时间
卡培他滨组和BSC组各有52位患者。中位随访了33.8个月后,卡培他滨组和BSC组分别发生了23例(44.2%)和37例(71.2%)进展或死亡事件。卡培他滨组的中位PFS明显长于BSC组:35.9个月 vs 8.2个月(风险比[HR] 0.44,p=0.002)。卡培他滨组的客观缓解率也较BSC组明显更高(25.0% vs 11.5%),缓解持续时间也明显更长(40.0个月 vs 13.2个月)。
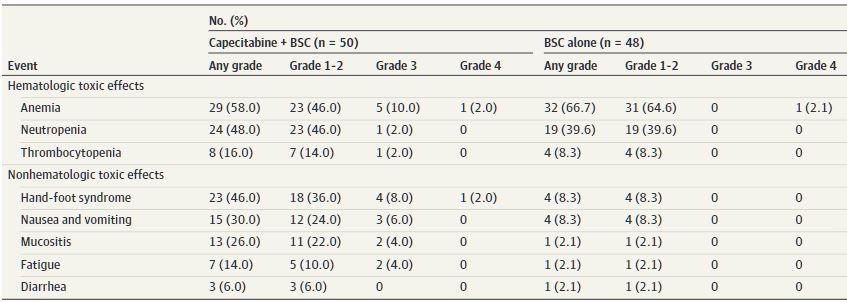
两组的不良反应事件
在维持治疗期间,最常见的3/4级不良反应事件有贫血(12.0%)、手足综合征(10.0%)、恶心和呕吐(6.0%)、疲劳(4.0%)和粘膜炎(4.0%)。无治疗相关死亡事件。
综上,对于经含卡培他滨方案诱导化疗后获得疾病控制的转移性鼻咽癌患者,卡培他滨维持治疗可显著延长无事件生存期,而且毒副作用可控。
原始出处:
Liu Guo-Ying,Li Wang-Zhong,Wang De-Shen et al. Effect of Capecitabine Maintenance Therapy Plus Best Supportive Care vs Best Supportive Care Alone on Progression-Free Survival Among Patients With Newly Diagnosed Metastatic Nasopharyngeal Carcinoma Who Had Received Induction Chemotherapy: A Phase 3 Randomized Clinical Trial.[J] .JAMA Oncol, 2022, https://doi.org/10.1001/jamaoncol.2021.7366
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Oncol#
68
#生存预后#
111
#卡培他滨#
85
#转移性#
55
好
71
此,建立一个基于患者表型或基因交
78