JCO:第一个多队列篮子试验——MyPathway初步研究结果发布
2018-01-15 肿瘤资讯编辑部 肿瘤资讯
随着二代测序的应用,越来越多低频突变被发现。因基因变异频率较低,如果采用传统的临床试验方式进行研究,很难达到统计学要求的样本量,为此,创新性的临床试验诞生——篮子试验和雨伞试验。
随着二代测序的应用,越来越多低频突变被发现。因基因变异频率较低,如果采用传统的临床试验方式进行研究,很难达到统计学要求的样本量,为此,创新性的临床试验诞生——篮子试验和雨伞试验。其中,MyPathway研究就是一个经典的多队列篮子试验。近日,《JCO》杂志发布了MyPathway研究的初步结果。
背景
目前,在肺癌,乳腺癌,结直肠癌和其他多种肿瘤中,根据患者的分子突变谱来选择靶向治疗药物已经成为临床常规。过去20年中,常见的有明确治疗效果的分子靶点包括HER2,EGFR,BRAF和Hedgehog通路。除了在已经获批相应靶向药物的肿瘤中检测到这些分子靶点的变异以外,其他瘤种中也可以检测到这些靶点,然而发生率通常较低(<5%),要对这些患者单独进行临床研究,很难满足传统研究的样本量要求。
篮子试验根据特定的基因变异将肿瘤进行分类,不限定原发肿瘤部位,使得靶向治疗用于相应基因变异成为可能。既往已经报道了几个小型的篮子试验,如vemurafenib用于BRAF V600突变的非黑色素瘤以外的其他实体瘤,显示出较好的治疗效果。这些研究结果提示,无论患者的肿瘤起源,携带特定基因突变是预测靶向药物治疗疗效的重要标志物。MyPathway是一个多中心的IIa期研究,含有多个队列的篮子试验。研究旨在评估相应靶向药物用于含有特定基因变异肿瘤的疗效(适应症以外的肿瘤)。评估的靶点和靶向药物包括:HER2(帕妥珠单抗+曲妥珠单抗),BRAF(vemurafenib),Hedgehog通路(vismodegib)和EGFR(厄洛替尼)。本研究报道了MyPathway试验中最初入组的可以评估疗效的230例患者。
方法
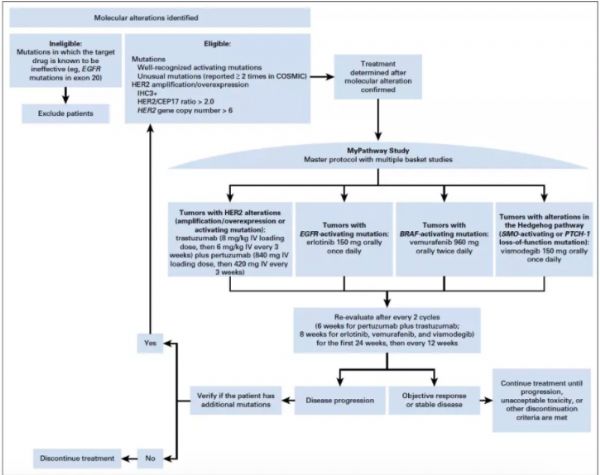
研究入组转移性实体瘤,含有以下任意靶点活化变异:HER2,EGFR,BRAF和Hedgehog pathway。若相应靶向药物已经获批用于某种类型的肿瘤,则患者不能入组。所有患者必须有可测量病灶,ECOG PS评分0-2分。Mypathway研究是一项多中心,非随机,开放的多队列篮子试验,研究设计如下图1。入组的患者必须含有以上任意一个靶点的活化变异,若患者携带两个或以上的基因变异,则有研究者确定最具有临床意义的靶点,进行相应的队列研究。含有HER2基因变异(扩增,突变或过表达)的患者接受帕妥珠单抗+曲妥珠单抗治疗;含有EGFR活化突变的患者接受厄洛替尼治疗;含有BRAF突变的患者接受vemurafenib治疗;Hedgehog通路变异的患者接受vismodegib治疗。研究的主要终点为客观缓解率ORR,次要终点包括疗效持续时间(DOR),无进展生存期,1年的OS率。
图1.研究设计
结果
从2014年4月1日至2016年11月1日,研究共入组了251例患者,覆盖35种不同的肿瘤类型,纳入本次疗效分析的患者230例,其余21例患者还未能进行第一次疗效评估。入组患者的中位年龄为62岁(范围)23-86岁,其中男性51%,91.6%的患者ECOG PS评分0-1分,既往接受过中位2.5个治疗方案。其中107例患者的分子变异是采用诊断时的肿瘤组织标本检测,其余123例患者是采用后续的活检标本进行分子检测。
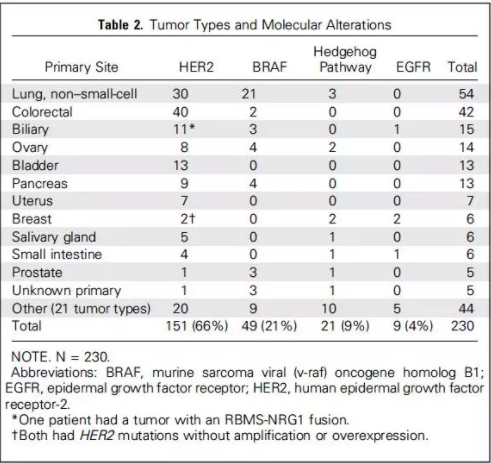
入组患者的肿瘤类型和分子变异情况总结见下表。230例患者,HER2变异的患者151例(66%),BRAF突变的患者49例(21%),Hedgehog通路活化的患者21例(9%),EGFR突变的患者9例(4%)。在151例进入HER2研究队列的患者中,114例为HER2扩增或过表达(其中12例同时检测到HER2突变),36例为HER2活化突变,另1例为RBMS-NRG1融合导致HER2通路活化。49例进入BRAF研究队列的患者,26例为BRAF V600E突变,其余23例为其他类型的BRAF活化突变。
疗效:
研究队列的中位随访时间为9.7个月,覆盖14种肿瘤的52例(23%)患者取得客观缓解,其中4例为CR,48例为PR;另外26例患者疗效评价为SD,疗效持续时间>120天。各个研究队列中均观察到取得客观缓解的患者。目前,各个研究队列均达到了最低疗效要求,只有BRAF突变队列中将不再入组BRAF非V600突变的患者(因为疗效较差,ORR为4%;1/23)。
HER2扩增/过表达的患者:
研究入组114例HER2扩增/过表达的患者,其中30例患者观察到客观疗效(2例CR,28例PR),ORR为26%(95%CI:19%-35%)。取得客观缓解的患者包括9种原发肿瘤类型:结直肠癌,膀胱癌,胆道癌,唾液腺癌,NSCLC,胰腺癌,卵巢癌,前列腺癌和皮肤癌,总结见下表。

在HER扩增/过表达队列中,最主要的肿瘤类型为转移性结直肠癌,共37例,这些患者既往接受过中位4线治疗,曲妥珠单抗+帕妥珠单抗治疗后取得PR的患者14例(38%;95%CI:23%-55%),4例患者为SD,疗效持续时间>120天,总结见下图2A。总体人群,中位DOR为11个月。在HER2变异队列中,尽管其他肿瘤类型的患者数目较少,也取得相对较好的疗效。其中,晚期膀胱癌患者的ORR为33%(1例CR患者疗效持续时间超过15个月,目前仍在获益;2例PR患者疗效持续时间分别为1个月和6个月),此外2例膀胱癌患者疗效为SD>120天,如下图2B所示。7例胆道癌,2例为PR(ORR为29%),3例为SD>120天,如下图2C。5例唾液腺癌,4例为PR(ORR为80%)。
HER2突变的患者:
36例HER2突变患者接受了曲妥珠单抗+帕妥珠单抗治疗,其中4例患者取得客观缓解,ORR为11%。其中14例为NSCLC,在NSCLC患者中,3例取得PR(ORR为21%),1例为SD>120天。其余22例其他肿瘤类型的患者,仅1例为PR(胆道癌)。
BRAF变异的患者:
BRAF V600突变的患者和其他类型BRAF变异的患者相比,疗效差异显著。26例BRAF V600突变(均为V600E突变)的患者,12例取得客观缓解(2例CR,10例PR;ORR为46%),覆盖6种不同类型肿瘤,总结见下表。相反,在23例非BRAF V600突变的患者中,仅1例取得了PR(ORR为4%,变异类型为CUX1-BRAF融合)。未观察到客观缓解的BRAF变异类型包括:K601E,G464V,G469A,G496A,N581S,G466V,G596R,G606E,L597Q,P731T,内含子9重排,内含子10重排,MACF1-和MASFL-BRAF融合。在BRAF V600E突变的患者中,NSCLC是最主要的肿瘤类型,共14例患者,其中6例患者取得客观缓解(1例CR,5例PR,2例为SD>120天;ORR为43%),见下图2D,中位DOR位5个月。
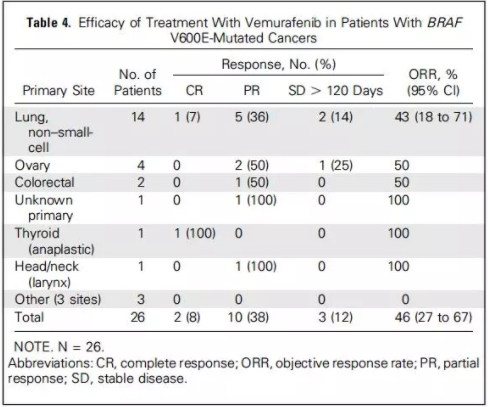

图2.HER扩增/过表达和BRAF突变患者的疗效瀑布图
Hedgehog通路活化或EGFR突变的患者:
共入组21例Hedgehog通路活化的患者(PTCH1突变的患者18例,SMO突变的患者3例),其中3例患者接受vismodegib治疗后取得PR(1例原发灶不明,1例为皮肤鳞癌,1例为唾液腺癌),这3例患者均为PTCH-1突变的患者。共入组9例EGFR突变的患者,其中1例取得PR(尿道腺癌)。
结论和讨论
MyPathway研究旨在含有HER2,BRAF,EGFR或Hedgehog通路活化的肿瘤患者中评估相应靶向治疗药物的疗效。从最初入组的230例患者的疗效数据来看,所有4个靶向治疗方案均观察到有意义的疗效,覆盖了14种不同类型的肿瘤,超出了药物目前获批的适应症范围。MyPathway研究还将继续招募患者,本次报道的数据,证实了这一研究的可行性以及篮子试验设计的潜在价值,为其他研究的设计提供参考。初步的研究结果提示,这4种获批的靶向治疗药物,在合并特定分子变异的其他类型肿瘤中也可以取得一定的疗效,如曲妥珠单抗+帕妥珠单抗用于HER2活化/过表达的结直肠癌,膀胱癌,胆道癌和唾液腺癌;vemurafenib用于BRAF V600E突变的NSCLC。目前,Mypathway研究还在继续,其他后续研究的结果。
原始出处:
John D. Hainsworth, et al. Targeted Therapy for Advanced Solid Tumors on the Basis of Molecular Profiles: Results From MyPathway, an Open-Label, Phase IIa Multiple Basket Study. Journal of Clinical Oncology. Jan 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#研究结果#
74
#pathway#
63
#JCO#
57
学习了谢谢分享!!
83
学习了谢谢分享!!
93